Introduction
The lack of local or muscle flap options for the lower leg and foot makes reconstructing defects in these locations challenging, often necessitating free flap surgery [1,2]. The vessels that supply blood to the lower extremities are also important sources of blood during lower extremity reconstruction. The popliteal artery arises from the femoral artery and divides into the anterior tibial artery (ATA) and tibial artery, and distally into the posterior tibial artery (PTA) and peroneal artery (PRA). At the anterior aspect of the ankle joint, the ATA becomes the dorsalis pedis artery [3-6]. The PTA divides into the medial and lateral plantar arteries, and at the foot level, the dorsalis pedis and lateral plantar arteries form the foot arch and provide circulation.
The PRA usually terminates in small branches that communicate with the anterior and posterior tibial arteries at the ankle joint level. In some cases, various congenital or acquired variations in the branching of the PRA occur. While the specific cause of the mutation leading to the congenital variations is unknown, it is no longer rare. Nonetheless, as changes in the arteries mentioned above can affect the success of leg and foot reconstruction, awareness of these changes is essential for successful surgery [7].
When a wound occurs in the middle area of the lower leg, a propeller flap or soleus flap can generally be tried for small and medium defects and a free flap for large defects. On the other hand, when a wound occurs on the foot, a distally based sural flap or free flap can be tried for small and medium-sized defects, and a free flap for large defects [1,7-9].
However, if the patient has vascular abnormalities, flap options should be carefully considered. Selection of the proximal flap becomes even more important when two flaps are required for one recipient artery; flaps that will not affect blood flow in the distal area must be chosen.
The patient we present had congenital ATA hypoplasia, suffered fourth-degree burns to the lower extremity from an electric blanket, and had soft tissue defects in two areas, requiring reconstruction. In this case, a free flap was most appropriate because large defects were located in the middle area of the lower leg and foot dorsum [1,8]. However, because blood flow was insufficient due to congenital ATA hypoplasia, we decided that a free flap might cause additional distal blood flow problems, and therefore chose to use a keystone perforator flap to reduce donor site morbidity. We introduce a case of reconstructive surgery using a keystone perforator flap, which we have found helpful for performing reconstructive surgery in patients with a congenital lower extremity vascular abnormality. The study was approved by the Institutional Review Board of Dongguk University Hospital (IRB No. 110757-202110-HR-05-02). The patient provided written informed consent for the publication and the use of his images.
Case
A 71-year-old man who was taking medication for hypertension, chronic obstructive pulmonary disease, and unstable angina was admitted to our hospital after suffering a contact burn to his right leg while sleeping on an electric blanket 2 days prior. The patient had no recollection of the burns at time of admission; we assumed they were caused by exposure to an excessively hot electric blanket for an extended time while sleeping. At admission, two burn wounds measuring approximately 12.0×6.0 cm and 12.0×10.0 cm, which corresponded to 3% of total body surface area, were observed on the right foot and right lower leg, respectively, with full skin layer necrosis and eschar formation (Fig. 1A).
Dressing treatment alone was deemed inadequate, so we decided to perform escharectomy 11 days after the burn injury. At surgery, necrotic changes were observed in part of the tibialis anterior muscle, and debridement was performed under a diagnosis of fourth-degree burns. Also, vacuum-assisted closure was applied for 2 weeks to reduce dead space before flap surgery (Fig. 1).
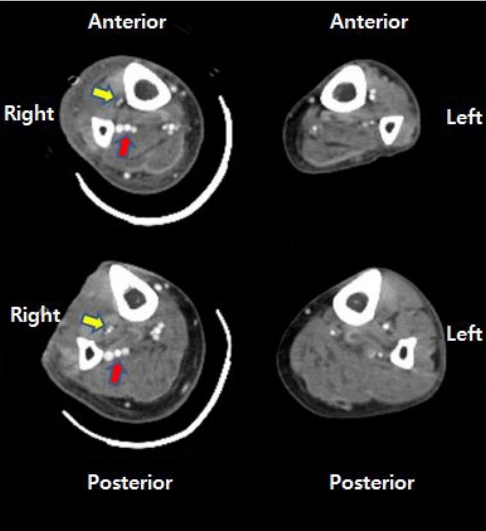
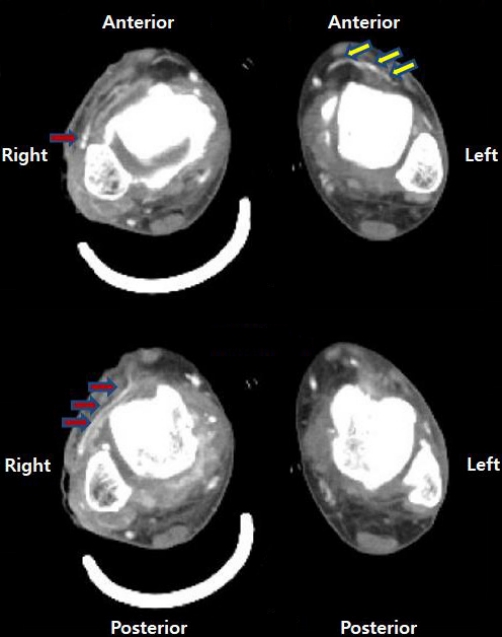
Afterwards, the flaps best suited to cover the defects were selected. Preoperative computed tomography (CT) angiography was performed to accurately evaluate the surgical sites, and ATA hypoplasia was observed, with blood supply to the dorsalis pedis artery from the PRA forming the pedal arch (type III-B) (Figs. 2, 3). Therefore, it was decided to treat the two burn wounds with perforator flaps. Peroneal perforators were found 13 to 18 cm above the lateral malleolus, where they emerged from the septum of the flexor hallucis longus and peroneus brevis muscles. A keystone-design perforator-based flap measuring 20.0×9.0 cm was marked over the lateral calf after three perforators were identified by Doppler. The flap was dissected in the subfascial layer based on the perforators, then elevated and advanced medially to cover the tibial wound. Afterwards, the path of the dorsalis pedis artery was marked with Doppler. A flap measuring 10.0×5.0 cm was designed based on the artery, and after dissection and elevation in the subfascial plane, the flap was advanced laterally to cover the instep. The donor site was covered with a split-thickness skin graft (Fig. 4).
About 8 months after surgery, no wound complications such as scar contracture occurred, and the patient could walk without restriction in joint movement (Fig. 5, Supplementary Video 1).
Discussion
Although knowledge of normal anatomy is a prerequisite when evaluating a patient before surgery, surgeons must also be aware of vascular variations. Among these variations, variants of the popliteal fossa vasculature were first classified in 1989 by Kim et al. [10]. The patterns consist of three primary types and 10 subtypes. Type I, which is the most common type, includes abnormalities in blood vessel branches below the knee joint, and type II includes abnormalities in blood vessels above the knee joint. On the other hand, vascular abnormalities such as aplasia and hypoplasia are classified as type III abnormalities [7,8].
From the viewpoint of reconstruction, type III abnormalities are the most important because hypoplasia or aplasia in the main branch is likely to cause lower extremity vascular insufficiency. As regards type III, type III-A corresponds to hypoplasia of the PTA and replacement of the distal popliteal artery with a large PRA, while type III-B corresponds to hypoplasia of the ATA and a large PRA that continues directly to the dorsalis pedis artery, and type III-C corresponds to hypoplasia of the posterior tibial and anterior tibial arteries and PRA connection to the foot arch [6-8].
Our patient had a type III-B pattern and two soft tissue defects requiring two flap reconstructions in the area supplied by the PRA [6,7]. Considering these anatomical patterns, a comprehensive surgical plan was made to reconstruct the patient’s soft tissue defects.
Reconstructive options for lower extremity defects depend on a variety of factors, including the patient’s vascular anatomy and the location and size of the defect. For large defects in the mid-lower region and foot, a free flap is usually attempted [1,5]. In this case, we decided to apply a perforator-based flap rather than a free flap to the proximal wound, and because the surrounding tissue was relatively thick and flexible, a PRA perforator-based keystone flap was used in the lower leg area, while a dorsalis pedis artery island flap was used in the dorsal foot area.
In addition to the surgical method we used in the proximal area, reconstruction using various types of free flaps could also be considered, employing end-to-side anastomosis, perforator-to-perforator anastomosis or flow-through perforator flaps. However, the surgical procedures of end-to-side anastomosis and flow-through anastomosis can risk compromising the major vessels. Perforator-to-perforator anastomosis requires a high level of technical skill encompassing super-microsurgical technique. Such surgical procedures involve long operating times and can cause significant donor-site morbidity and scarring.
We chose the keystone flap for reconstructing the lower leg because it has several advantages over free flaps: for example, keystone flaps provide good color matching and are technically easier to achieve faster reconstruction of contour defects. Furthermore, recovery is better and quicker. For these reasons, the keystone flap is often performed for large defects in the lower extremity soft tissue [1,5,11].
In conclusion, we recommend a perforator keystone flap because it can produce good results and rapid recovery without wound complications. Furthermore, perforator keystone flap surgery can reduce donor site morbidity and leave fewer scars, which results in higher patient satisfaction. Lastly, we recommend preoperative angiography CT for wounds deep enough to warrant consideration of flap coverage, and stress the importance of surgery planning based on patient anatomy, as this is the factor that has the greatest impact on outcomes.
Few options exist for the coverage of large defects in the lower extremities. Though the typical choice is to use free flaps, we urge surgeons to consider other options. In the described case, the authors thoroughly examined available options and ultimately decided on a perforator keystone flap for reconstruction.