Introduction
A circumferential skin and softtissue defect in two adjacent fingers are challenging for any reconstructive surgeon. Moreover, circumferential defects after burn injuries are relatively rarer than partial injuries, because people tend to quickly withdraw on reflex from the source of injury. Although free flap surgery is widely used for such defects, other options should be considered if it fails or is not feasible. The groin flap, which was first described by Smith et al. in 1972 [1], is a reliable flap for reconstructing various body parts. Though several modifications of groin flaps for hand and finger reconstructions have been reported, there have been no publications on its application in a circumferential softtissue defect with bone exposure in two adjacent fingers [2,3]. Herein we present a case where a newly designed tubed-groin flap was applied to reconstruct a circumferential defect in two adjacent fingers. The patient provided written informed consent for the publication of this report and all accompanying images.
Case
A 22-year-old male with major depressive disorder suffered from severe electrical burns in his left index and middle fingers. He had wrapped his left index and middle finger with uncoated electric wires and plugged the wires into a 220-voltage outlet for about 30 minutes.
When the patient arrived at the emergency department 5 hours after injury, he had skin necrosis with circumferential eschar formation on his left index and middle fingers. The fingertips were spared, but necrosis ran from the proximal interphalangeal joints to the distal phalanges. Blood flow in the fingertips was not observed. A capillary filling test was attempted but was not validated. A pinprick test was subsequently performed on the fingertips using a 19-gauge needle but no bleeding was observed (Fig. 1). Except for the injured fingers which were the entry site, there were no clinical symptoms such as numbness or pain in the rest of the fingers, palm or forearm. There were also no identifiable exit wounds on either foot. Additional tests such as electrocardiography, complete blood count, electrolyte levels, serum myoglobin, blood urea nitrogen, serum creatinine and urinalysis for the evaluation of heart and kidney damage showed no specific findings. The patient immediately underwent escharectomy to reduce the in-terstitial pressure, which could cause ischemia and further necrosis by tissue edema. Unfortunately, the wound continued to aggravate over time (Fig. 2). The entire distal phalanx and surrounding tissues of the middle phalanx with exposed tendons were necrotized with bone exposure and periosteal injury, necessitating an ostectomy at the midpoint of the middle phalangeal bone. Furthermore, tenosynovitis occurred at 7 days in the flexor tendon of the index finger, necessitating further incision of the distal palmar crease (Fig. 3).
Fig. 1.
Postburn photographs on the day of injury. Dorsal (A) and palmar (B) views on admission. Eschar formation was observed on the burned skin.

Fig. 2.
Wound necrosis continued. Dorsal (A) and palmar (B) views 2 days after escharectomy and debridement.
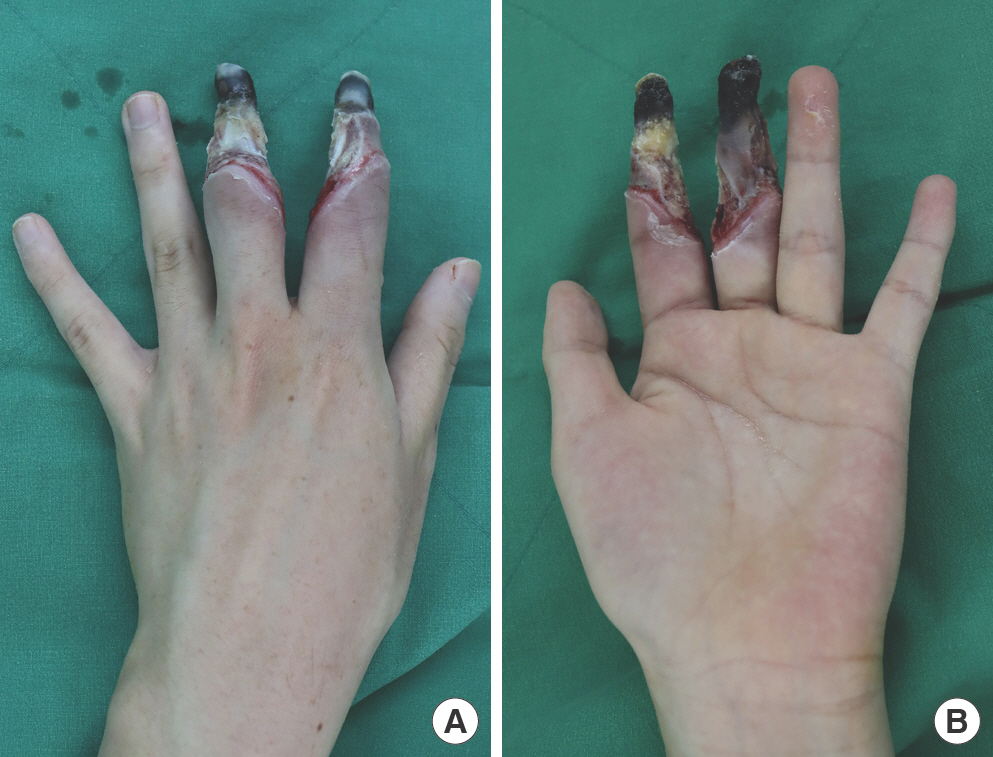
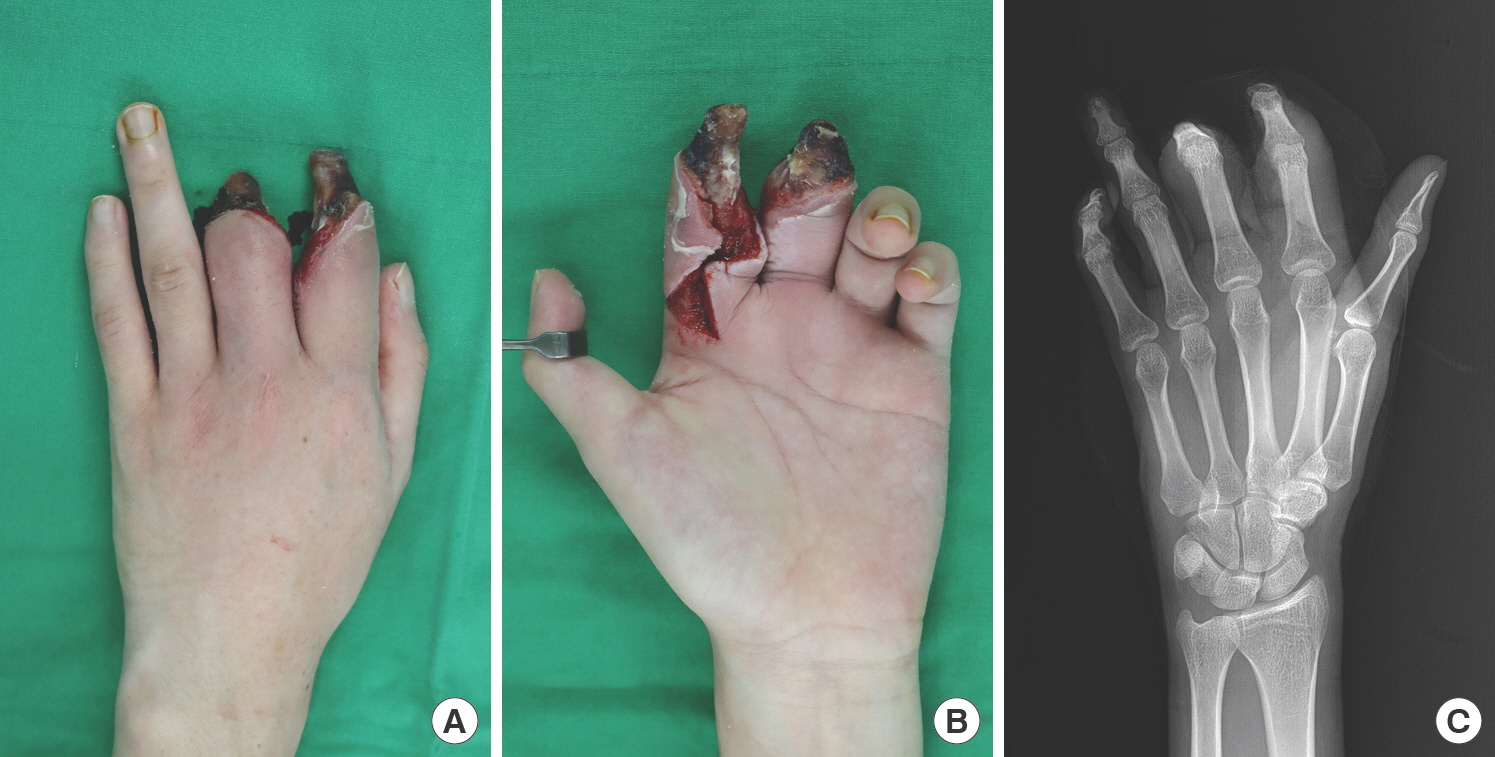
Fig. 3.
Necrosis progressed further. Dorsal (A), palmar (B), and X-ray (C) views after ostectomy and tenosynovitis incision.
Amputation of the digits at the metacarpophalangeal joint level was not considered since the patient and his parents insisted on preserving the length of the fingers. After serial debridement, reconstruction was performed using an anterolateral thigh perforator-based free flap to cover the defect on both fingers at 15 days after admission. An end-to-end anastomosis was performed to the common digital artery and dorsal metacarpal vein. Seventy-two hours after the operation, venous congestion was noted (Fig. 4). To salvage the flap, venous reanastomosis and vein graft interposition were carried out. However, venous thrombosis continuously occurred after several minutes. We opted to discontinue the salvage procedure and to perform an alternative flap instead.
Fig. 4.
Venous congestion occurred in the anterolateral thigh free flap. Dorsal (A) and palmar (B) views.

A pedicled groin flap was opted for because we believed that the failure of the free flap was due to vascular injuries on the recipient area. Another free flap with a longer pedicle was not considered due to patient opposition and risk of failure.
At 25 days after admission, secondary reconstruction was performed. A 7.5×8-cm-sized ipsilateral pedicled groin flap was designed and elevated to sufficiently cover the exposed bones of the left index and middle fingers, resulting in provisional syndactyly. After flap elevation by conventional method and excision of excessive fat, the distal part of the elevated flap was sutured to the proximal part of the flap site to create two holes for finger insertion. The index finger was inserted into the medial hole, and the middle finger was inserted into the lateral hole. For future division of syndactyly, a bolster suture was performed in the middle of the elevated flap (Figs. 5, 6).
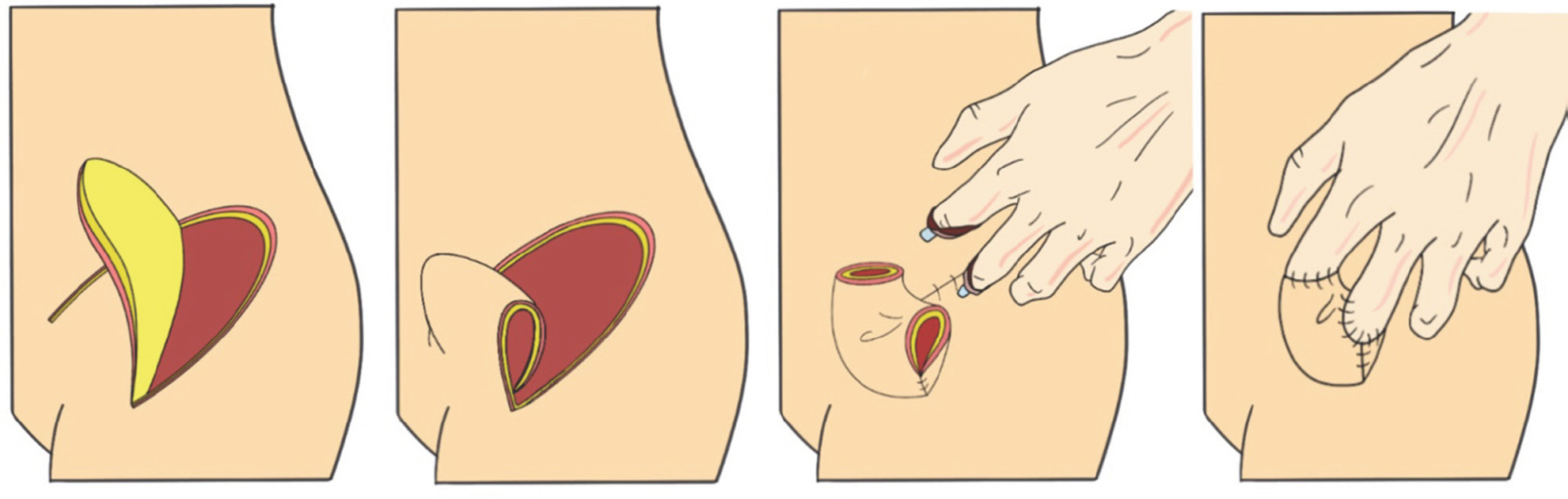
Fig. 6.
Schematic view of the surgical technique. After elevation of the groin flap, the distal part was sutured to the proximal part of the flap to make two holes. The two fingers were inserted in the holes respectively.
The donor site was closed directly, and the groin flap survived without any complications during follow-up. The flap was surgically delayed twice on postoperative days 16 and 19 after flap circulation was checked by rubber band compression. Flap detachment and closure of the remaining donor site were performed on postoperative day 21 (Fig. 7). A syndactyly separation of the index and middle fingers was performed 2 weeks after the flap detachment. The skin flap was sufficient, so a skin graft was not needed on the ulnar side of the index finger or the radial side of the middle finger (Fig. 8).
Fig. 7.
Flap division. On postoperative day 21, the flap was detached from the inguinal area, and the tip was primarily closed. Dorsal (A) and palmar (B) views.
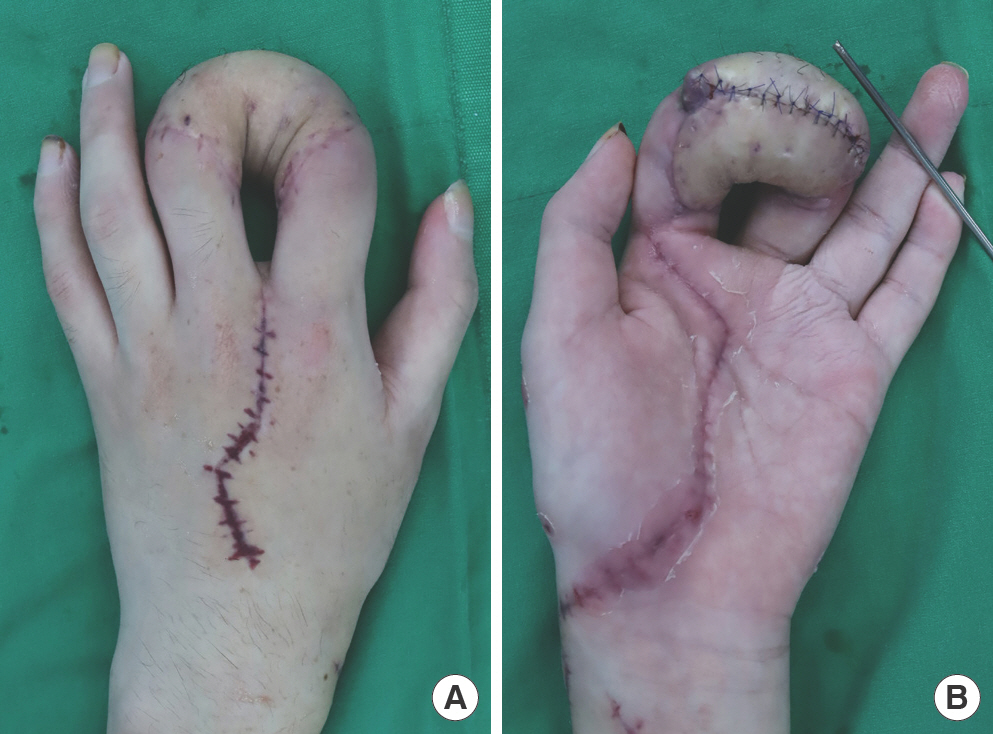
Fig. 8.
Syndactyly separation. At 14 days after detachment, the separation of syndactyly was performed between the two fingers. Dorsal (A) and palmar (B) views.

There were no complications during the 8 months follow-up period. The patient was satisfied with the well-reconstructed fingers, which showed adequate length and function. A debulking procedure could be required later. A full range of motion of the metacarpophalangeal joints was restored during re-habilitation. The patient could now grasp and pinch objects using his index and middle fingers (Fig. 9). However, the lack of sensation on the tips of the fingers which were subjected to trauma impede delicate work on the part of the patient, and remain a shortcoming.
Discussion
Thermal burns are classified into four levels according to depth of penetration from the epithelial surface into the tissue. Epidermal (superficial) burns which involve the epidermis and superficial partial-thickness burns involving the epidermis and part of the papillary dermis are usually treated conservatively and do not require surgery. In deep partial-thick-ness burns, which involve the entire papillary dermis down to reticular dermis, excision and skin graft is considered in some cases such as large areas, or highly mobile or cosmetically sensitive areas. However, full-thickness burns involving all layers of the dermis and underlying deeper tissues require surgical intervention. Moreover, if full-thickness burns caused by electricity are found in extremities, treatment becomes more complicated as the muscles, tendons, bones, and vessels can be affected, thereby leading to necrosis and amputation.
The reconstruction of deeply burned fingers is a rare and challenging problem for reconstructive surgeons because the fingers require functional and favorable aesthetic outcomes to perform daily activities and to allow the patient to resume their normal lives [4,5].
Recently, free flaps have been used mainly for reconstructing large hand defects. The anterolateral thigh free flap is used most commonly, while other flaps, such as the medial sural artery perforator, radial forearm, and lateral arm free flap, can also be used depending on the size and location of the defect [6]. However, in case the free flap fails, surgeons should consider another option to cover the defect.
The groin flap, which was described by Smith et al. in 1972 [1], is an axialpattern flap based on the superficial circumflex iliac arteriovenous system. Since its introduction, it has been widely used for softtissue coverage of the fingers, hands, and distal forearms. Although it has several disadvantages, including the need for flap division and occasional debulking surgery, patient discomfort, and prolonged hospital stay, the groin flap also has many advantages, such as versatility, relatively quick application and easy technique, the fact that it does not require microsurgical techniques, and lower donor site morbidity compared with free flaps. Furthermore, it can also be used in patients with vascular injuries [7,8].
Several modifications and innovative procedures of the groin flap for finger reconstruction have been documented. However, most of them were for defects on one finger or a partial defect on multiple fingers. To our knowledge, only few cases have been reported on circumferential defects in two adjacent fingers with bone exposure that were reconstructed using a groin flap.
Although an abdominal flap can be used for multiple finger defects like our case, it was not considered due to the visible scar formation on the donor site.
When a surgeon encounters a patient with a circumferential softtissue defect with distal phalangeal bone exposure in two adjacent fingers and considers a pedicled groin flap, the surgeon would most likely wrap the two adjacent fingers trans-versely or horizontally. In cases where this technique was employed, additional skin graft surgery with a long-term risk of contracture is inevitable after division surgery.
Therefore, we present a newly designed groin flap for coverage of two adjacent fingers. After conventional flap elevation and tube shape formation, the center of the tube-shaped flap was bended into a natural curve and each finger was inserted into either the ensuing medial or lateral holes. This ensured the two fingers were not attached to each other, and the center of the bended curve formed an imaginary line for future finger division. Additionally, a bolster suture was performed between the two distal sides of the fingers. A skin graft was not needed because of the abundance of skin flaps between the two fingers. Our method can also be applied not only to adjacent fingers but to non-adjacent fingers, with appropriate modifications. Likewise, it can be applied to the abdominal flap, and is helpful when a groin flap is contraindicated.
Herein, we report a successful case of tubed-groin flap for a circumferential defect in two adjacent fingers after failure of a free flap. One regret is that we had not assessed the vascularity in the electric burn patient before the free flap, which led to free flap failure, prolonged hospital stay and additional surgery and with involvement of another donor site.
We believe that our design of groin flap can be a reliable and convenient solution for the reconstruction of two adjacent fingers when a free flap fails or is not indicated. Furthermore, our method has advantages in that skin graft surgery is not required at syndactyly separation, and that it can also be applied to abdominal flaps and between other non-adjacent fingers.

















