Introduction
Preauricular sinus, also known as a preauricular pit or ear pit, is a congenital malformation characterized by a small pit or sinus located near the front of the ear, resulting from the incomplete fusion of the first and second branchial arches during embryonic development. It is a relatively common condition, with a reported prevalence of 0.1% to 0.9% in various populations [1]. In most cases, preauricular sinuses remain asymptomatic, but they can occasionally become infected, leading to abscess formation. When promptly managed, they usually respond well to conservative treatment such as antibiotics and local wound care. However, some neglected cases can result in the extension of infection to nearby structures, leading to severe complications such as pinna, external auditory canal, temporomandibular joint, and scalp involvement [2]. Here, we present a case of a neglected preauricular sinus abscess that extended to the adjacent scalp area, causing significant complications and management challenges. This report aims to discuss the clinical presentation, diagnostic approach, treatment modalities, and potential complications associated with such an unusual and severe presentation. The study was approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (IRB No. 2023-07-019). The informed consent was waived.
Case
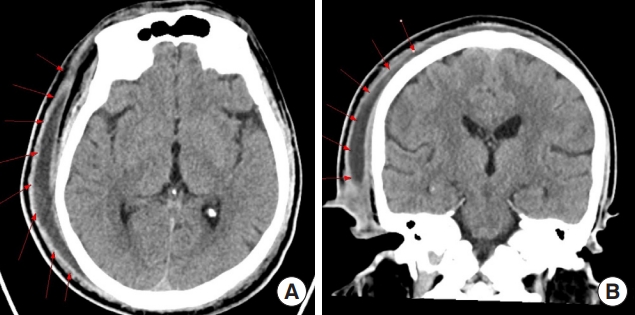
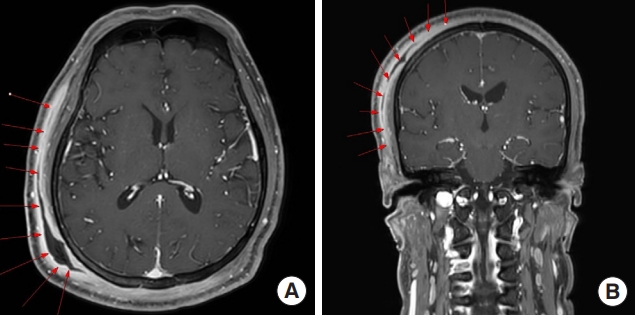
A 42-year-old male patient, with a history of a right preauricular sinus diagnosed at our hospital in 2001, presented through the emergency room with mental changes in December 2022. Though the patient was diagnosed with diabetes in 2019, he scarcely adhered to medication and remained in a state of unregulated blood glucose levels. Previously, inflammation of the right preauricularfistula had improved and then exacerbated repeatedly and intermittently. His general condition had been gradually deteriorating over the past month, followed by inability to leave his house and difficulty in mobility as a result of increasing muscle weakness of the entire body. Emergency brain computed tomography revealed an extensive abscess formation involving the postauricular area of the right ear and the entire right scalp (Fig. 1). A 2×1 cm-sized abscess opening at the right postauricular area was identified, with opaque and yellowish discharge emanating from the opening (Fig. 2). The lab test results at the emergency room showed a white blood cell count of 52.1×10³/μL, indicating leukocytosis. C-reactive protein (CRP) was measured at 300 mg/dL, and procalcitonin at 6.62 ng/mL, suggesting a severe inflammation. Additionally, the initial blood sugar test was 500 mg/dL, and hemoglobin A1c was 12.5%, indicating poor blood sugar control, accompanied by ketonuria and ketoacidosis. Consequently, the diagnosis was diabetic ketoacidosis (DKA). The deterioration in the patient’s general condition and the altered mental state were attributed to poor control of pre-existing high blood glucose levels, compounded by the development of a severe inflammation leading to the formation of a large abscess, ultimately resulting in DKA.
Management and treatment
When the patient presented to the emergency room, ceftriaxone antibiotics were administered. The initial intervention involved an incision and drainage as the primary therapeutic measures, and a pus culture was conducted, which detected Staphylococcus epidermidis. In conjunction with the culture examination, the antibiotic susceptibility test revealed resistance to penicillin and macrolides. Consulting with the infectious disease medicine department, vancomycin and piperacillin/tazobactam antibiotics were administered throughout a 1-week hospitalization period. During the hospitalization period, aseptic dressings and wound irrigation were performed daily. Additionally, hydration and insulin therapy were administered, resulting in the improvement of the patient’s mental status and the normalization of blood glucose levels. However, inpatient treatment became impractical due to the patient’s personal circumstances. The patient was discharged, and subsequent treatment through outpatient care was planned. Though daily outpatient wound dressing was provided, even after 3 weeks, there was no sign of improvement in the wound. Consequently, the patient was referred to the plastic surgery department for appropriate management of widespread infectious wounds. Magnetic resonance imaging (MRI) confirmed the presence of necrotizing soft tissue inflammation and abscess formation in a wide range of areas across the right temporal and parietal regions of the scalp (Fig. 3). A surgical plan for total resection (en bloc resection) of necrotizing tissue and reconstruction using an ipsilateral latissimus dorsi (LD)-free flap was developed. In spite of the surgical plan, immediate debridement in the operative room could not be performed due to the patient’s personal circumstances. Instead, the following treatments were undertaken. To prepare the patient for surgery and ensure suitable conditions, proactive daily dressing changes and bed-side debridement were performed. We also administered antibiotics to control initial inflammation. Oral amoxicillin/clavulanate potassium antibiotics were maintained for 2 months. During this period, three outpatient cultures performed at 2-week intervals did not identify any specific pathogens. After 2 months of continuous and repeated treatments, the wound demonstrated significant removal of necrotic tissue, revealing a fresh wound bed, leading to the decision for hospitalization for surgery. Furthermore, through a follow-up examination conducted in mid-February, it was possible to confirm that the patient’s CRP level had normalized to 2.12 mg/dL, indicating sufficient inflammation control.
Surgical procedure
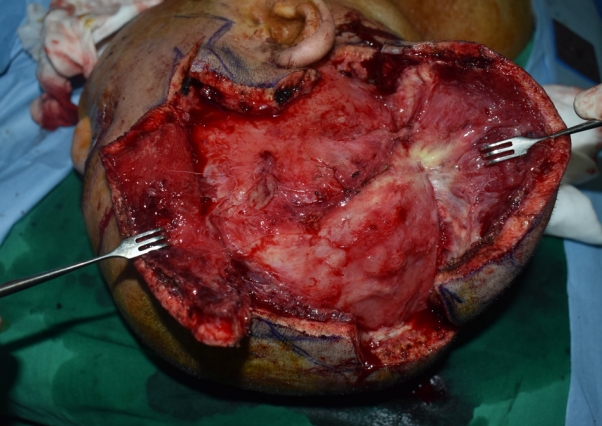
Under general anesthesia, an incision was designed and applied over the parietal scalp to perform en bloc resection to the depth of the periosteum. Necrotizing infected tissues were confirmed at the entire right scalp area (Fig. 4). Debridement was performed over an area of approximately 12×12 cm, extending about 12 cm upward from the right ear, about 5 cm forward from the ear, and about 7 cm backward from the ear. All inflammatory tissues were meticulously removed, and pus was drained from the affected areas (Fig. 5). During the excision, partial skin preservation was performed, and upon approximation, the final defect size measured 4.5×11.5 cm. A 5×16 cm-sized ipsilateral LD-free flap was used for reconstruction, with anastomosis of thoracodorsal artery to facial artery and vena comitans to external jugular vein (Fig. 6).
Postoperative course and follow-up
The duration of hospitalization for surgery and postoperative care totaled 30 days. Upon readmission for surgery, a tissue culture performed in the operating room revealed the presence of carbapenem-resistant Acinetobacter baumannii. Postoperatively, ampicillin/sulbactam and tigecycline antibiotics were administered throughout the hospitalization period. All hemovac drains were removed on the 14th-day post-surgery (Fig. 7). Aseptic dressing was consistently maintained at the surgical site during the 2-week hospitalization period from postoperative day 14 to day 29, and the patient was eventually discharged without any complications. During 6 months of outpatient clinic follow-up, there was no recurrence of inflammation at the surgical site, nor complications such as seroma or hematoma (Fig. 8). The patient also expressed satisfaction with both functional and cosmetic outcomes.
Discussion
Preauricular sinus is a congenital opening commonly located at the anterior margin of the ascending limb of the helix. The prevalence of this condition ranges from 0.1% to 0.9%, and it follows an autosomal dominant inheritance pattern characterized by incomplete penetrance and variable expression. It may also be linked to other congenital anomalies like hearing loss or renal disorders, as seen in cases of Branchiootorenal syndrome. The prevailing theory behind the development of a preauricular sinus attributes it to the incomplete or defective fusion of the six auditory hillocks during auricle development. The occurrence of preauricular sinuses can be either sporadic or inherited. More than half of the cases are unilateral, typically occurring sporadically. Bilateral occurrences are more likely to be inherited, although incomplete autosomal dominance with reduced penetrance is common, accounting for nearly 85% of the cases [3]. Most preauricular sinuses remain asymptomatic. However, in cases of pit infection, it can lead to the formation of a discharging sinus or abscess. Recurrent infections may result in cellulitis, perichondritis, and the formation of hypertrophic scars.
When symptoms appear, most cases can be resolved by using appropriate antibiotics that match the cultured bacterial strain. Therefore, proper antibiotic use through bacterial strain culture is essential. Also for patients requiring surgery, it is necessary to prioritize inflammation control through antibiotic use, as there are risks of bleeding, recurrence, and post-surgical complications in cases of severe inflammation.
In cases of recurrent inflammation, certain types of bacterial strains, such as Staphylococcus and Enterobacter, were found to be associated with higher recurrence rates when identified from wound cultures in culturing [4]. Therefore, when Staphylococcus or Enterobacter strains are identified during the initial strain testing, it can be assumed recurrence is highly likely, possibly calling for more aggressive surgery. Patients with a history of recurrent inflammation should undergo surgical treatment. If the sinus tract is not completely excised and remains, recurrence is highly likely. To avoid missing minor branches of the tract, probes or methylene blue dye may be used for staining. Regarding tracking and completely excising the tracts, some authors argue that microscopic surgery is superior to the previous methods. However, this approach requires sophisticated equipment and surgical expertise, which reduce cost-effectiveness and hinder broad application [5]. In extensive abscess surgery originating from the preauricular sinus, reducing the recurrence rate is of utmost importance. En bloc excision can be a favorable solution to remove all branches of complex tracts through a simpler procedure. In cases like ours, where the abscess has spread extensively to adjacent tissues, preventing recurrence becomes even more essential.
To ensure complete excision, it is crucial to establish appropriate surgical planes. The surgical approach is based on the following anatomical considerations: the development of congenital preauricular fistula occurs when the auricular primordium of the first and second branchial arch have incomplete nodule fusion [6]. Through histological and embryonic analysis, it can be inferred that the fistula base is typically situated within the subcutaneous tissue, residing between the superficial layer of the temporal fascia and the auricular perichondrium. The soft tissue anterior to the tragus and helix crus is devoid of critical nerves, major blood vessels, or vital organs, except for the arteria temporalis superficialis and the auriculotemporal nerve. Even when these structures are ligated or injured, they have minimal impact on the blood supply and muscle function of the head and face. Consequently, performing an en bloc resection of the fistula base poses no significant risk of adverse effects on the morphology and function of the local area. In our case, the presence of Staphylococcus strains confirmed during the initial strain testing, along with a history of recurrent infections and improvement, were strong indications for surgery. Probes were not used in the surgical field, while methylene blue dye was employed to visually identify and remove a wide-ranging abscess that extended to the scalp, as seen on the preoperative MRI. Depending on the extent of the initial abscess, en bloc excision may result in extensive defects; reconstruction with minimal dead space can require a significant amount of tissue. It should be noted that without sufficient tissue, there is possibility of recurring inflammation. Therefore, accurately assessing the extent of the abscess before surgery and planning the reconstruction accordingly is crucial. In our case, we were able to obtain sufficient tissue by using an ipsilateral LD-free flap.
Preauricular sinus is a common congenital anomaly, and in most cases, is often overlooked and not reported unless there are symptoms or complications such as the formation of abscesses. However, in some cases, abscesses can spread extensively to surrounding tissues and even present with systemic symptoms. In rare instances, as in our case, the abscess can extend to the scalp, leading to life-threatening complications, such as impaired consciousness. Therefore, when preauricular sinus abscess becomes recurrent despite repeated conservative treatments, potential risks should be considered. In our case, we first controlled the inflammation with appropriate intravenous antibiotics and then proceeded with en bloc excision. This approach simplified the surgical process, minimized the risk of missing minor branches, and reduced the probability of recurrence, leading to satisfactory outcomes after surgery.
We report this case to highlight the importance of recognizing the potential risks associated with recurrent preauricular sinus abscesses and the successful results achieved by implementing a systematic approach combining conservative treatment and surgical intervention.