Introduction
Perianal defects after tumor resection are often diverse and complicated. They refer to circular defects on the perianal region despite preservation of the anal sphincter. Reconstruction of these defects is challenging because three-dimensional reconstruction techniques are often required. With inappropriate treatment, contracture and scarring can impede normal anal function; therefore, the skin graft technique is not recommended in this region. Several flaps have been introduced for reconstructing this region, including the V-Y advancement flap, gluteal thigh flap, and inguinal flap [1-5]. However, the described flaps are thick and cannot make the natural structure of the superficial mucosa over the anal sphincter. For physiologic and natural reconstruction of the anal and perianal region, a much thinner flap is required. Additionally, considering the anal passage, a circular structure is required to prevent scar contracture.
In general, when performing surgery on the perineal area, temporary colostomy is often necessary to prevent delayed wound healing, infection, and abscess formation due to fecal contamination [6]. However, if simple and proper circular lining around the anus is reconstructed, these complications from fecal contamination can be minimized and temporary colostomy can be avoided. In this report, we present an anal reconstruction case using a bilateral angel wing flap which provided a natural conduit. Thanks to the simplicity of the operation, colostomy diversion was not required. The study was approved for exemption by the Institutional Review Board of Hanyang University Hospital
(IRB exemption No. 2022-12-045) and informed consent for publication of the study was obtained from the patient.
Case
A 44-year-old woman with no underlying diseases underwent a biopsy for a nodular mass on the anal margin, which was diagnosed as squamous cell carcinoma. The biopsy results showed a 1.4×1.2 cm-sized invasive squamous cell carcinoma in the 11 to 1 o’clock direction and 4×3 cm-sized squamous cell carcinoma in situ in all other directions, with a depth of invasion limited to the reticular dermis at 3 mm, corresponding to T2 stage (8th American Joint Committee on Cancer). There was no sphincter muscle involvement, lymphovascular invasion or metastasis; thus the cancer was classified as stage I (T2N0M0). Therefore, transanal excision was performed without neoadjuvant chemotherapy or radiotherapy.
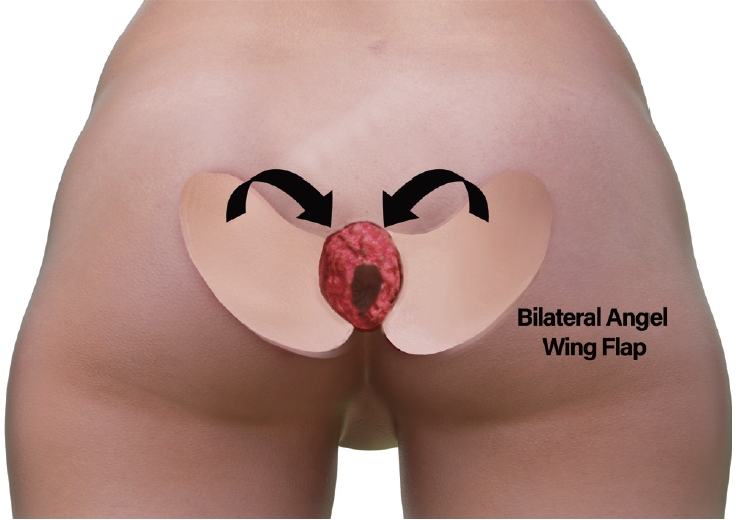
After resection of the affected area including anal skin and mucosa, the total defect size was about 8×6 cm (Fig. 1A). A portable Doppler device was utilized to identify perforators within the perianal area. Perforators closest to the defect were chosen, and the edge of the flap was planned in close proximity to the defect. The long axis of the flap was arranged in parallel with the infragluteal fold axis. The flap length, determined from the distance between the perforator and the distal flap margin, was designed to be slightly longer than the defect itself. The flap width was designed to match the broadest width of the defect, which was assessed from the inner anal mucosal edge to the skin border. The “angel wing” configuration was designed at the upper margin of the flap, which was integrated into the neo-anal mucosal lining (Fig. 2). The flap was harvested in a distoproximal direction at the avascular plane of the suprafascial level. Caution was exercised near the perforators in the proximal one-third of the flap. However, no extensive dissection was necessary around the perforators to skeletonize them. Dissection continued until an adequate arc of rotation was attained without entirely isolating the pedicle. A similar approach was employed for the design of the contralateral side. After elevating flaps of 3×5.5 cm, each flap was transposed to the defect, and the “angel wing” margin of the flap was first inset to the neo-anus mucosal lining by medial rotation (Fig. 1B). Then, the donor site was closed easily without tension (Fig. 1C) [7]. It was believed that complications from fecal contamination would be minimal because the perianal defect was adequately lined by the angel wing flap. Therefore, no additional temporary colostomy was performed. Instead, a low-residue diet was maintained for 1 week after surgery to delay defecation as much as possible, and dressings were changed immediately in case of any fecal contamination at the surgical site.
There was no complication such as flap necrosis, infection, seroma or wound disruption. Also, during the long-term follow-up of 2 years, according to medical history taking and digital rectal examination, the patient did not have any passage problems including incontinence or webbing scar contractures (Fig. 3).
Discussion
To reconstruct the anal passage, classically a bilateral V-Y advancement flap has been used [4]. However, this flap is a two-dimensional reconstruction method which does not take into account the depth of the anal tract defect. Because of that, the V-Y advancement flap is likely to flatten the anus, resulting in webbing contracture of the conjoined flap area and inevitable incontinence after reconstruction [4,5]. For this reason, physiologic reconstructions should be considered for the three-dimensional anal tract structures, including anal mucosal lining and skin lining.
The thickness of the flap is also an important factor in anal reconstruction. A thick flap is not suitable for tailoring the flap inset around the anus area, as it may increase the risk of obstruction of the anal passage due to inappropriately large flap volume. Recently, the inferior gluteal thigh region has been noted because of its thinness, providing a particularly thin donor site for perforator flaps. However, at least for anal tract reconstruction, we believe the thigh perforator flap is still unsuitably thick because the flap cannot be used to make superficial circular structure such as the inner anal passage tracts, and is better suited for unilateral or outer perianal region reconstruction.
For making natural anus passage tracts, we believe that adjacent anal soft tissues are the most suitable and sufficiently thin structures, minimally affected by sex, age, body mass index, and race. The anus and perianal skin area receive a rich vascular supply from the superior gluteal, inferior gluteal, and internal pudendal arteries. Numerous perforators arise from these arteries; therefore, designing the flap is relatively simple and easy when based on perianal perforators. We have had numerous experiences with angel wing flaps for vaginal and sacral reconstruction [7]. These experiences can be applied around the anal area because of the rich vascular and perforator networks. This perforator-based island flap is simple because there is no need for skeletonization around the perforator pedicle. We saved only the proximal one-third of the flap pedicle area, which still achieved a sufficient arc of rotation. The operative scar is minimal in hidden areas such as the infragluteal fold. This short scar itself not only reduces the operation time (about less than 1 hour), but also makes a temporary colostomy unnecessary by reducing the possible area of fecal contamination. Though this study did not include a large number of patients, the technique is a representative and educational model for all surgeons, including those in colorectal and reconstructive fields.
Perianal defects can have various causes, such as anal cancer, chronic abscess, autoimmune ulcers, and Fournier’s gangrene. The method of reconstruction for such defects determines the patient’s quality of life [8]. Because anal passage problems can easily arise from postoperative perianal scar contracture, inadequate flap thickness, and lack of contribution to three-dimensionality, perianal reconstruction is challenging for many surgeons. As one solution to this problem, we introduced our anal reconstruction technique using a perforator-based island flap. This “angel wing” flap would be a good option for improving the patient’s quality of life.