 |
 |

|
| Aims and Scope |
| About the Journal |
| About the Society (KWMS) |
| Editorial Board |
| Open Access |
| Principles of Transparency and Best Practice |
| Editorial Office |
| Subscriptions |


|
| Aims and Scope |
| About the Journal |
| About the Society (KWMS) |
| Editorial Board |
| Open Access |
| Principles of Transparency and Best Practice |
| Editorial Office |
| Subscriptions |

AbstractOur case highlights a 41-year-old male with a past medical history of severe diverticular disease since age 30, diabetes mellitus type 2, hypertension, protein calorie malnourishment, and body mass index of 50 kg/m2 who presented for a large bowel obstruction. Active surgical issues included: chronic incisional hernia, enterocutaneous fistulae, and a megacolon secondary to a recto-sigmoid anastomotic stricture. In collaboration with a colorectal surgeon and by using a multimodal approach, we successfully addressed the patient’s gastrointestinal issues and incisional hernia. The multimodal approach included botulinum toxin A (BTA) injections to the abdominal wall flat muscles (external oblique, internal oblique, and transverse abdominus), installation of an abdominal reapproximation anchor (ABRA) dynamic tissue system (DTS), and porcine urinary bladder matrix (PUBM) xenografts. The patient received BTA injections prior to the index operation, which lasted over 12 hours. The ABRA DTS assisted in achieving primary fascial closures. Definitive closure of this class 4 wound was facilitated by the antimicrobial and accelerated wound healing properties of PUBM as well as a unique multimodal approach to achieve exemplary results in a patient with multiple complex surgical issues.
IntroductionChronic incisional hernia with loss of domain (LOD), enterocutaneous fistulae, and megacolon are complex surgical issues, any one of which is difficult to manage alone [1]. After the index operation, during which a large abdominal exposure is necessary for appropriate management of these pathologies, definitive closure of the abdomen may not be possible due to patient instability [2,3]. Failure to appropriately close the abdomen can both lead to bowel damage, recurrent herniation, and a need for skin grafting [2,4-6]. Therefore, achieving early primary fascial closure after repair of incisional hernia with LOD is very important for patient’s long-term quality of life.
Historically, temporary abdominal closure techniques have included the Bogota bag and the static traction closure Wittmann Patch [3,4,7,8]. Negative pressure therapy (NPWT) systems, such as AbThera (KCI USA), are a recent addition to the surgeon’s toolbox that should only be used as a bridge to definitive closure. Botulinum toxin A (BTA) injections can be used concurrently with AbThera to relax the abdominal flat muscles. The abdominal reapproximation anchor (ABRA, Canica Design Inc.) dynamic tissue system (DTS) allows for successful closure of the catastrophic open abdomen, largely by acting as a “faux linea alba” and can be used in conjunction with the above tools to achieve primary fascial closure. The reestablished linea alba restores a biomechanically functional abdominal wall. This aids in myofascial closure by providing dynamic tension that gradually facilitates relaxation of the rectus myofascial units, allowing the myofascial gap (MFG), defined as distance between the medial edges of the rectus muscles, to decrease over time [2,5,9]. Finally, porcine urinary bladder matrix (PUBM) xenografts–which provide an intact basement membrane scaffold comprised of the inner two layers of the porcine bladder, collagen, growth factors, glycosaminoglycan, and other proteins–are assistive technologies that can both accelerate wound healing and achieve full wound closure in difficult-to-close wounds [9,10].
Here we present a unique case of a super morbidly obese patient with a chronic incisional hernia with LOD, multiple enterocutaneous fistulae, and a chronic megacolon that was successfully managed via a multi-specialty, multimodal approach utilizing a combination of BTA, NPWT (AbThera), ABRA DTS, and PUBM. Our institution does not require ethical approval for reporting individual cases or case series. Written informed consent was obtained from the patient for anonymized information to be published in this article.
CaseA 41-year-old male with a past medical history of severe diverticular disease since age 30, type 2 diabetes, hypertension, depression, alcohol abuse, and super morbid obesity (body mass index [BMI] of 50 kg/m2) was admitted for worsening abdominal pain, nausea, and vomiting. The patient had an extensive surgical history relating to severe diverticulitis. He required an emergency exploratory laparotomy, sigmoidectomy, and Hartmann’s procedure for perforated diverticulitis in his early thirties. Four years later, following an elective exploratory laparotomy, the patient developed an incisional hernia with LOD, multiple enterocutaneous fistulae, and a megacolon.
On admission, the initial focus was medical and nutritional optimization. On hospital day 5, the patient received 300 units of BTA injection into the bilateral flat muscles to chemically paralyze and relax the muscles. Injection was done as a bedside procedure in sterile fashion with 50 units of BTA injected into each muscle (e.g., external oblique) of the flat muscles bilaterally using ultrasound guidance. Once medically and nutritionally optimized, the patient underwent the corrective index operation on hospital day 16. The index operation, performed by the colorectal surgeon, included an exploratory laparotomy, extensive lysis of adhesions, and resection of the obstructing colorectal stricture, concluding in a total abdominal colectomy with end ileostomy (Fig. 1A). In addition, three segmental small bowel resections with side-to-side stapled anastomoses were necessary to address the three enterocutaneous fistulae (Fig. 1B). The abdominal wall closure team then conducted the initial assessments and application of the AbThera NPWT. The initial myofascial defect included: MFG 50 cm, length 30 cm, visceral extrusion (VE) 6 cm (Fig. 2), whereby VE is defined as the extrusion of visceral contents above the posterior fascia. The patient was cared for in the surgical intensive care unit and was on a nil per os diet receiving total parenteral nutrition with goals of early enteral feeding. On postoperative day (POD) 3, the patient was returned to the operating room for an open cholecystectomy due to chronic cholecystitis, and ABRA DTS installation. Upon completion of the ABRA DTS installation, the MFG (which had decreased to 30 cm) further decreased to 17 cm and VE to 0 cm. His course was complicated by a retroperitoneal hematoma that was successfully coil embolized. The patient was re-explored without deinstallation of the ABRA DTS to ensure there was not an intraabdominal component to the hemorrhage. On POD 21, it was determined that he was not ready for ABRA DTS deinstallation. Fractured elastomers, secondary to the prior re-exploration, were replaced and elastomer adjustments were performed. The maximal MFG at ABRA DTS replacement and adjustment was 4.5 cm. The patient’s progression on ABRA DTS is best captured in Fig. 3. On POD 26, the patient underwent ABRA DTS deinstallation and primary incisional herniorrhaphy closure to complete the recreation of the linea alba. The incisional herniorrhaphy closure employed the bidirectional Smead-Jones technique with 22-#2 Vicryl on a TP1 needle, and NPWT was placed over the surgical site. On POD 31, the patient was returned to the operating room for examination under anesthesia during which the primary incisional herniorrhaphy was noted to be intact. Subsequently, an onlay hernioplasty with PUBM, vertical panniculectomy with umbilectomy, and complex plastic surgical wound closure was performed. Computed tomography imaging obtained 3.5 months postoperatively (Fig. 4) revealed no evidence of recurrent incisional hernia. At the follow-up wound assessment meeting, the patient had very well closed wounds with positive healing (Fig. 5).
DiscussionThis case report demonstrates a multi-specialty, multimodal approach to successfully managing the combination of a chronic incisional hernia with LOD, multiple enterocutaneous fistulae, and a megacolon using BTA, NPWT, ABRA, and xenografts. Studies by Haddock et al. [7] and Okullo et al. [5] document closure of morbidly obese patients using ABRA, but the patient presented in this case study had both a greater BMI (50 kg/m2), larger MFG (50 cm), and a more extensive surgical history. Lastly, our patient’s wound area was 1,500 cm2, an area much larger than those reported by Salman et al. (374 cm2), Yetisir et al. (468 cm2), and even Long et al. (575.9 cm2) [3,6,11]. In this incredibly complicated surgical scenario, successful primary fascial closure was achieved using BTA, NPWT, DTS, and PUBM.
BTA injections, one of the components of the multimodal approach, block presynaptic acetylcholine release to cause muscle relaxation and elongation of abdominal muscles. These injections have been widely used for many purposes in abdominal closure, with most success in cases of ventral hernia repair [12]. Our institution, with its extensive experience successfully closing large chronic incisional hernias with LOD, uses BTA injections for their efficacy in relaxing the flat muscles prior to performing planned surgical procedures. The paralysis peaks at 2–4 weeks and its effects can last up to 6–9 weeks [13,14].
The ABRA DTS allows for successful closure of the catastrophic open abdomen and is an important tool in this case report. By acting as a faux linea alba, the ABRA DTS reestablishes a biomechanically functional abdominal wall, which aids in myofascial closure by providing dynamic tension that gradually decreases the MFG [4,5,9]. It is installed using a series of elastomers extending through the full thickness of the abdominal wall, anchored to buttons flanking the myofascial defect bilaterally. Elastomer adjustments interspersed with osteopathic maneuvers achieve proper dynamic tension, defined as 1.5 to 2 times stretch of the black tension markings across the MFG. With subsequent adjustments and corresponding osteopathic maneuvers over time, the ABRA DTS dynamically decreases the MFG [9]. ABRA DTS is an easier-to-use and more effective system than mesh imbrication or sequential suturing [1,4]. Common complications of the ABRA procedure include pressure sores at button sites, enteroatmospheric fistulae, and ventral hernias [4,5,15]. However, many studies have noted a surprising lack of fistula formation and ventral hernia development [2,5,8,11,15]. Many of the failures of ABRA noted in literature are attributed to device disruption by either patient or another pathology that require deinstallation of the system rather than failure of the system itself [5]. We hypothesize that these failures may also be secondary to over-tightening of elastomers, leading to elastomer fractures. At our institution, close attention to the feel of the elastomer for adjustment termination has likely contributed to a nearly 0% elastomer fracture rate [9].
NPWT, another component of the multimodal approach, was efficacious for various reasons. The AbThera is a bridge to definitive primary myofascial closure and protects the viscera in the open abdomen scenario. Additionally, NPWT and DTS have a synergistic effect on wound healing. Placement of NPWT over the ABRA DTS reduces edema and drains any exudate, thus protecting the skin [2,4,5,7-9]. Wang et al. [8] noted that in a cohort of 47 trauma patients, 12 patients of whom received both ABRA placement and NPWT, 100% achieved closure. Similar closure success rates have been reported widely in the literature [1,4,8,11,15]. In contrast, the NPWT only cohort required more surgeries (2.0 vs. 2.5) and had a lower closure success rate of 28%.
PUBM xenografts, the final component of the multimodal approach, are assistive technologies consisting of a basement membrane for scaffolding, collagen, growth factors, glycosaminoglycans, and other cell signaling proteins that facilitate and accelerate wound healing. These products come in the form of powder or sheets and are used by surgeons and wound care specialists to accelerate wound healing and achieve full wound closure in a variety of wounds. Furthermore, xenografts have antimicrobial properties that can facilitate wound healing while minimizing risk of surgical site infection [9,10]. This is particularly important in this case study of class 4 dirty-infected wound.
Our case emphasizes the importance of a multi-specialty, multimodal approach in addressing the multiple concurrent surgical issues presented in this case. The use of BTA and NPWT early in the patients’ surgical course allowed for the MFG to decrease from 50 to 30 cm. Further use of the ABRA in conjunction with previous modalities led to definite fascial closure. Furthermore, the prompt use of the multimodal approach led to better outcomes in our patient. Therefore, we recommend the multimodal approach outlined in this case report that include the use of BTA injections, ABRA DTS, NPWT, and PUBM to successfully manage complex surgical patients.
Fig. 1.Initial clinical photographs. (A) Large megacolon removed from the patient along with the large enterocutaneous fistulaes resected. (B) Multiple enterocutaneous fistulae. 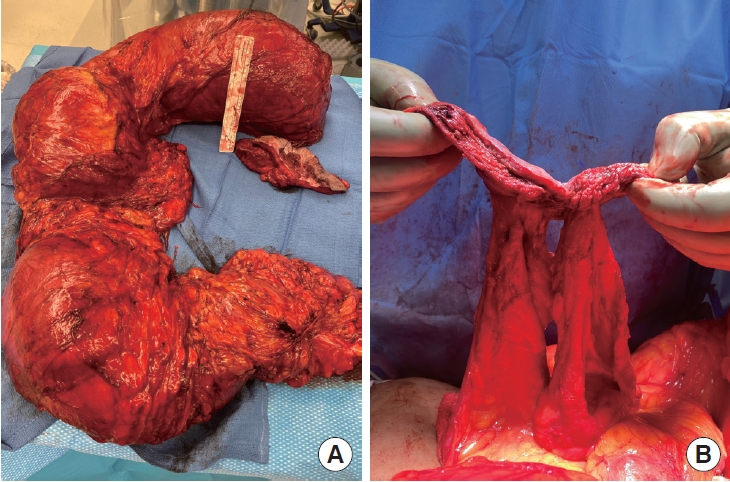
Fig. 2.Initial surgical photographs. (A) Large open abdominal wound. (B) Temporary cover of the large abdominal wound. 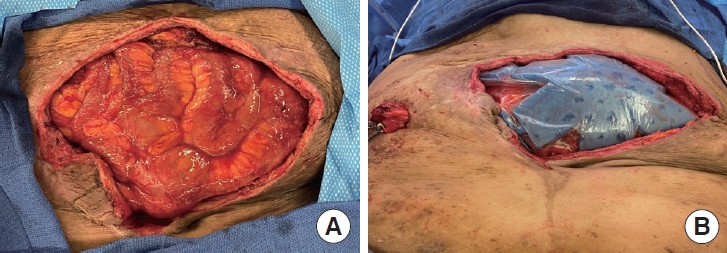
Fig. 3.Use of abdominal reapproximation anchor (ABRA) system. (A) Patient’s abdomen prior to surgical intervention. (B) ABRA system application. (C) Completion of abdominal wall reconstruction. (D) Myofascial gap during deinstallation of the ABRA system. (E) Myofascial closure completed, linea alba reconstructed. 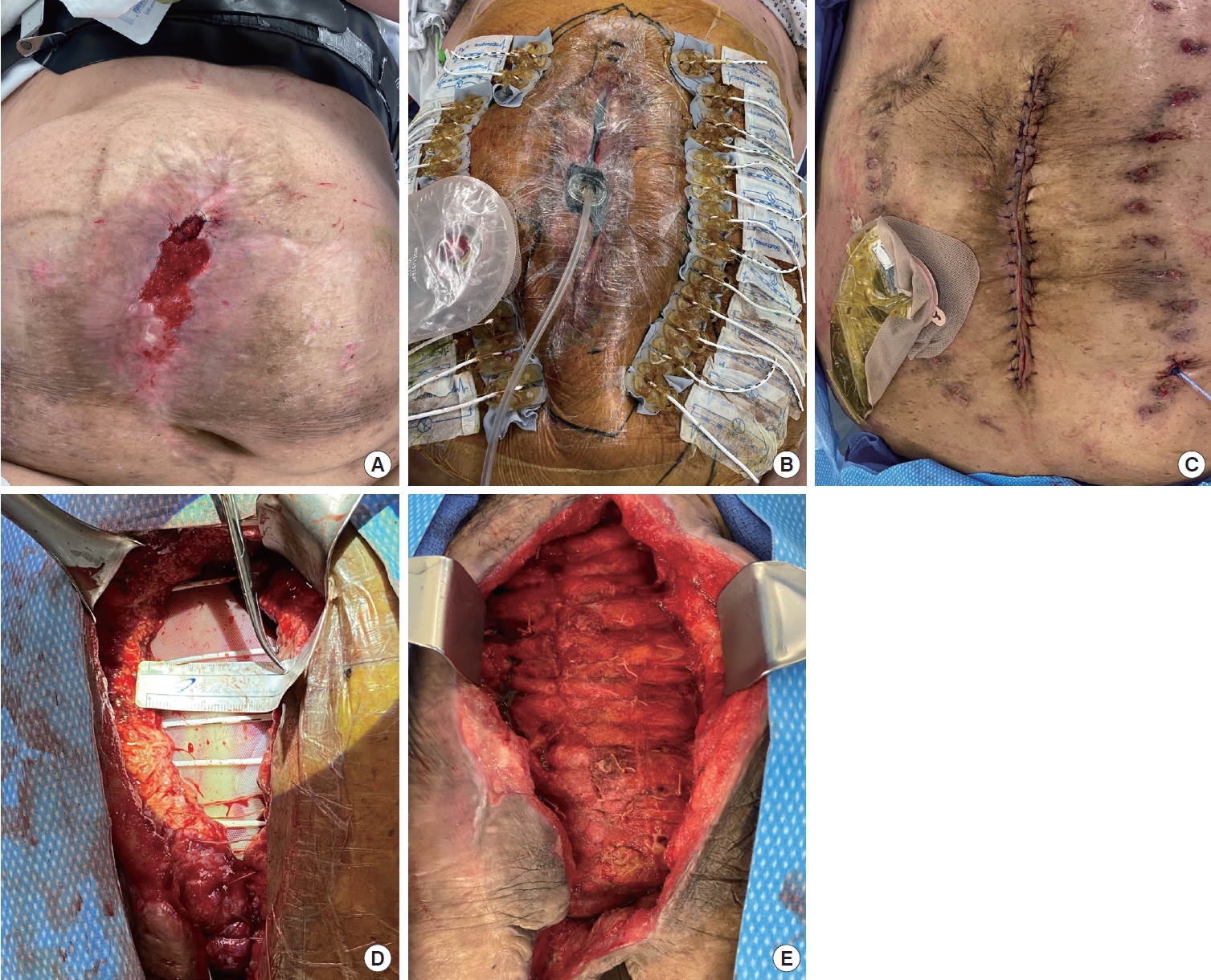
References1. Poortmans N, Berrevoet F. Dynamic closure techniques for treatment of an open abdomen: an update. Hernia 2020;24:325-31.
2. Reimer MW, Yelle JD, Reitsma B, et al. Management of open abdominal wounds with a dynamic fascial closure system. Can J Surg 2008;51:209-14.
3. Long KL, Hamilton DA, Davenport DL, et al. A prospective, controlled evaluation of the abdominal reapproximation anchor abdominal wall closure system in combination with VAC therapy compared with VAC alone in the management of an open abdomen. Am Surg 2014;80:567-71.
4. Mukhi AN, Minor S. Management of the open abdomen using combination therapy with ABRA and ABThera systems. Can J Surg 2014;57:314-9.
5. Okullo A, Siriwardhane M, Pang TC, et al. The abdominal reapproximation anchor device. Surg Innov 2017;24:49-54.
6. Yetisir F, Salman AE, Mamedov R, et al. Intrarectal negative pressure system in the management of open abdomen with colorectal fistula: a case report. Int J Surg Case Rep 2014;5:164-8.
7. Haddock C, Konkin DE, Blair NP. Management of the open abdomen with the abdominal reapproximation anchor dynamic fascial closure system. Am J Surg 2013;205:528-33.
8. Wang Y, Alnumay A, Paradis T, et al. Management of open abdomen after trauma laparotomy: a comparative analysis of dynamic fascial traction and negative pressure wound therapy systems. World J Surg 2019;43:3044-50.
9. Puckett Y, Caballero B, Tran V, et al. A case series of successful abdominal closure utilizing a novel technique combining a mechanical closure system with a biologic xenograft that accelerates wound healing. J Vis Exp 2019 Jul 4 [Epub]. https://doi.org/10.3791/57154.
10. Lecheminant J, Field C. Porcine urinary bladder matrix: a retrospective study and establishment of protocol. J Wound Care 2012;21:476-82.
11. Salman AE, Yetisir F, Aksoy M, et al. Use of dynamic wound closure system in conjunction with vacuum-assisted closure therapy in delayed closure of open abdomen. Hernia 2014;18:99-104.
12. Farooque F, Jacombs AS, Roussos E, et al. Preoperative abdominal muscle elongation with botulinum toxin A for complex incisional ventral hernia repair. ANZ J Surg 2016;86:79-83.
13. Catalan-Garza V, Pena-Soria MJ, Saez-Carlin P, et al. Long-term results of botulinum toxin type A in complex abdominal wall repair and review of the literature. Updates Surg 2020;72:1201-6.
14. Mourad AP, De Robles MS, Winn RD. Low-dose pre-operative botulinum toxin a effectively facilitates complex ventral hernia repair: a case report and review of the literature. Medicina (Kaunas) 2020;57:14.
15. Chen N, McLaren M, Slater K. The abdominal re-approximation anchor device (ABRA®) has the potential to be useful in both emergency and elective dynamic temporary fascial closure. ANZ J Surg 2020;90:2456-62.
|
|