Introduction
Necrotizing fasciitis of the genital and perianal tissues resulting from urologic and colorectal infections is known as Fournier's gangrene. The disease can progress ag-gressively and become lethal. Fournier's gangrene often passes through deep fascial planes of the penis, scrotum, perineum, and lower abdomen. Initial treatment of Fournier's gangrene includes wide and radical debridement of infectious tissues to control the infection. Hence, most cases require perineoscrotal reconstruction after primary treatment [1,2]. However, Fournier's gangrene rarely extends upward into the high intermuscular plane, especially into the supralevator plane in the anal region [3], because the fascial planes of the sphincteric area are distinguished from the periscrotal area.
Herein, we present our experience managing a very rare case of high intersphincteric abscess with Fournier's gangrene in a patient with perianal infection, and successful reconstruction of the consequent extensive perianal defect using a perforator-based island flap. The patient provided written informed consent for submission and publication of this report and accompanying images.
Case
A 63-year-old non-insulin-dependent diabetic male sought evaluation in our emergency room for severe pain and swelling of the scrotum. He had experienced painful discharge around the anus for 1 week. An abdominal computed tomography scan revealed air collection in the scrotum, penis, and perineum, consistent with a diagnosis of Fournier's gangrene (Fig. 1). The infection probably originated from the perianal region. However, no definite abscess around the intersphincteric region was noted on the initial examination. Emergency ultrasound-guided drainage of the perineal abscess was performed with simultaneous radical debridement. The penis and scrotal infections were initially controlled by incision and drainage. However, the anal infection required serial drainage, debridement, antibiotics, and colostomy (Fig. 2A). The initial empirical antibiotic treatment began with ciprofloxacin after the first debridement. The patient was referred to the Plastic and Reconstructive department for infection control and reconstruction of the post-debridement defect around the anus. The wound was stable after the fifth serial debridement; hence, a vacuum-assisted wound closure system (VAC; KCI Medical, San Antonio, TX, USA) was applied (Fig. 2B and C). Unfortu-nately, the anal sphincter was already damaged. The defect in-volved the perianal region and inferior aspect of the scrotum (Fig. 2D). At the fifth debridement, methicillin-resistant Staphylococcus aureus was identified in the wound swab culture, and vancomycin was initiated. To cover the anus and inferior aspect of scrotum, we fashioned a 15x7cm perforator-based island flap. The posterior superior iliac spine and coccyx were designated as landmarks of the lateral sacral border along which many reliable perforators were found (Fig. 2E). A suitable perforator was selected near the defect using hand Dop-pler, and the flap design was adjacent to the tissue defect. The flap was subsequently elevated disto-proximally in the subfascial layer (Fig. 2F). During elevation of the proximal portion of the flap, great care was taken around the perforator pedicle, leaving undissected tissue of approximately 1-cm radius. Perforator skeletonization was not performed. We provided a sufficient angle of rotation with minimal dissection near the pedicle and the elevated flap was transferred easily. The long flap covered the inferior aspect of the scrotum and anus. The donor site was closed directly (Fig. 2G and H). Suction drain was removed 10 days after flap surgery. Until 6 weeks after surgery, both lateral positions were maintained to prevent the flap from being compressed. Antibiotics were administered from the first debridement to 3 weeks after flap surgery. As the sphincter was removed due to severe initial infection around the perianal area, the colostomy was permanently maintained. The patient had healed well without any complications at the 6-month follow-up (Fig. 2I).
Fig. 1.
Abdominal computed tomography scan. Computed tomography shows air collection in the scrotum, penis, and perineum, consistent with Fournier's gangrene.
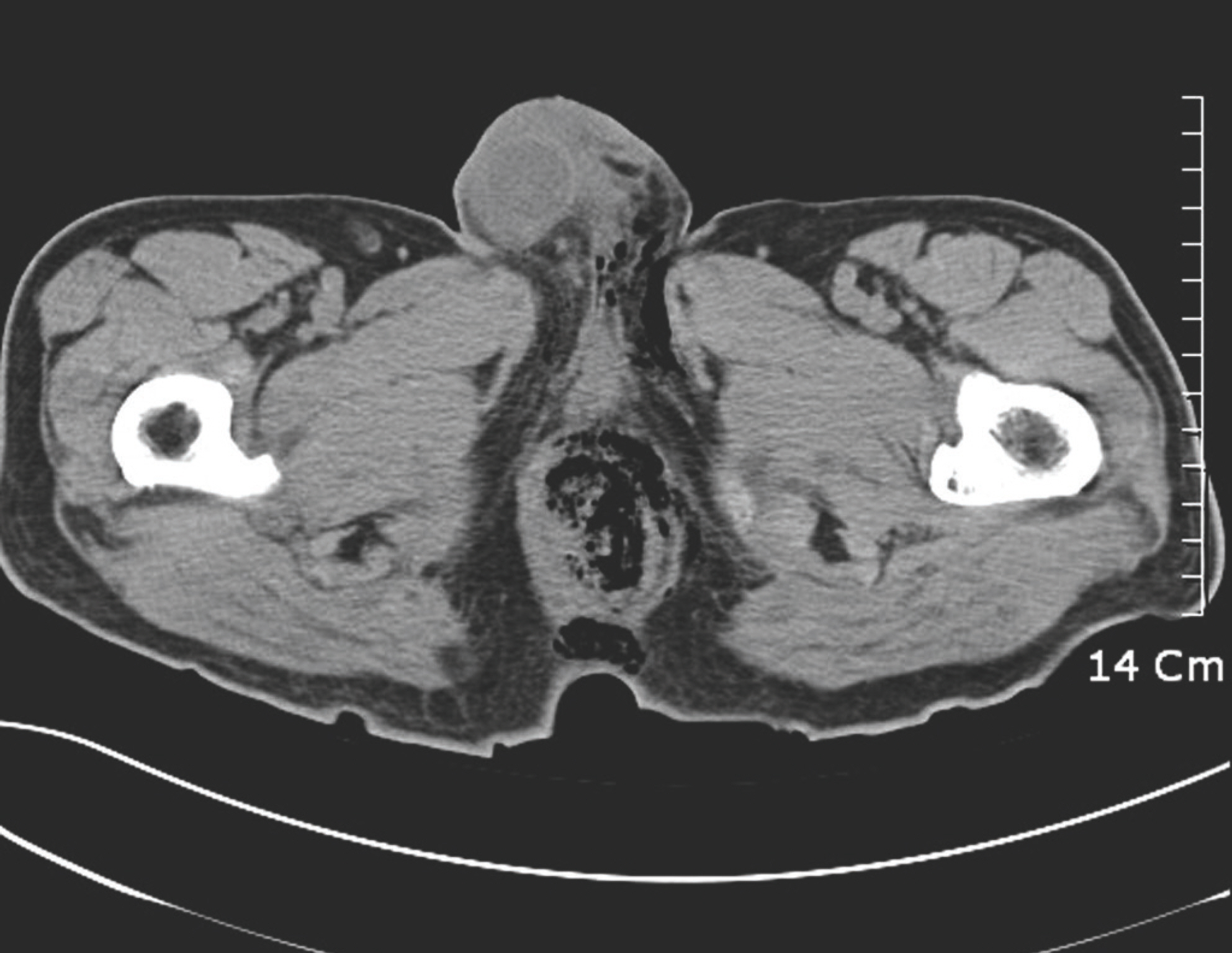
Fig. 2.
Reconstruction of the perianal defect using a perforator-based island flap. (A) Penis and scrotal infections are initially controlled by incision and drainage; however, the anal infection is not susceptible to the treatment. (B) Initial post-debridement photo representing the damaged lower anal sphincter; at this point, anal function is retained. (C) Anal sphincter and muscle are damaged severely after the fifth serial debridement and the wound is quiescent after which a vacuum-assisted wound closure system (VAC; KCI Medical) is applied. (D) The defect is visible in the perianal region and inferior aspect of the scrotum. The opening of the anus is already closed. (E) Posterior superior iliac spine and coccyx are marked and serve as surface landmarks of the lateral sacral border. We designed a 15×7 cm perforator-based island flap, which is elongated into the gluteal sulcus. (F) The flap is then elevated disto-proximally in the subfascial layer. Great care is taken near the perforator pedicle, leaving a 1-cm radius of undissected tissue. (G) The flap is transferred easily without pedicle perforator isolation. The donor site is closed directly. (H) Immediate postoperative view showing a thin and well-contoured flap to the anus and inferior aspect of the scrotum. (I) Patient had healed well without any complications at the 6-month fol-low-up.

Discussion
Fournier's gangrene is a soft tissue infection around the perineum that rapidly spreads into surrounding tissues [1,2]. Delays in diagnosis are common, owing to vague symptoms, resulting in sepsis and a high mortality rate [4]. To stabilize this invasive disease, serial debridement of infected tissues is needed, often leading to large defects of the perineal region. Reconstruction is difficult concerning aesthetics and function. Fortunately, ascending infection of anal structures and perianal regions are very rare in Fournier's gangrene. Hence, re-cent literature has highlighted the importance of periscrotal and abdominal reconstruction [5,6]. Numerous flaps, including superomedial thigh skin [1], anterolateral thigh [5], and gracilis myofasciocutaneous flaps [6] have been utilized for reconstruction of the periscrotal region. However, in our case, the perianal defect was more serious than the periscrotal defect because of uncontrolled infection from the lower perianal abscess. For cases of periscrotal reconstruction in Fournier's gangrene, a skin graft is often used [7]; however, in this case, a method that could provide sufficient volume to cover the perianal defect was required. Free flap surgery could have been an option [8], but it may have been difficult to perform microsur-gery after finding an appropriate healthy recipient vessel in this patient, who had a wide range of infectious soft tissue. To cover the anal region and inferior aspect of the scrotum, the posterior buttock tissues are suitable for a perforator-based is-land flap because they are rich in vascularity and have sufficient flap volume.
Recently, a need for flaps that allow for more options and customization in design while sparing muscle has arisen, resulting in the establishment of the perforator flap concept. With this new technique, clinicians can obtain flaps of larger dimensions compared with conventional musculocutaneous flaps; therefore, the perforator flap has become a more popu-larized and favored method where perforators are present. Buttocks have redundant perforators from the lumbar, superior gluteal, lateral sacral, inferior gluteal, and internal pudendal arteries, as described by Koshima et al. [9]. There are numerous constant and reliable perforators along the lateral sacral border. Numerous cases have reported the successful use of gluteal artery perforator flaps for large lumbosacral defect reconstruction with primary closure of donor sites [9,10]. However, the thick fatty tissue of the buttocks cannot be rendered as thin as periscrotal tissues. Besides, concerns arise regarding pedicle injury and postoperative compression of the vascular pedicle.
With perforator-based island flaps, these potential vascular problems are prevented by stopping flap elevation at the level of the perforator without trans-muscular dissection toward the proximal source vessel. Meticulous dissection or skeletonization of the perforator is not required if the elevated flap can move freely into the defective area without tension pivoting on a tissue pedicle surrounding the perforator [11]. The source artery is not important because the proximal portion of the flap pedicle along the lateral sacral border includes numerous “microperforators.” To overcome the disadvantages of thick, fatty gluteal tissues, the distal portion of the flap design was elongated to the gluteal sulcus or superior portion of posterior thigh where the skin flap is thin as the periscrotal region with similar skin characteristics. Vascular perfusion in the distal part of the flap is not an issue as undissected tissue is maintained at the proximal portion of the flap.
Since Fournier's gangrene is an aggressive infectious disease, active debridement in the early stages of the disease is essen-tial. For defects resulting from debridement, especially in cases involving a perianal defect, our new method is more convenient and safer compared to other perforator flap techniques as it can ensure abundant blood flow and sufficient volume. Therefore, the posterior buttock perforator-based island flap is a good option for reconstruction of Fournier's gangrene as it can successfully cover a defect involving the perianal region and inferior aspect of the scrotum.















