Introduction
Nonsuicidal self-injury (NSSI) is defined as an act with the purpose of hurting one-self without a clear suicidal intent [1]. The mechanisms of NSSI include a range of behaviors such as cutting, burning, scalding, hair pulling, banging body parts, self-poi-soning, and scratching [2]. Although rates vary among studies, the lifetime prevalence of NSSI is approximately 4% in the adult population, and up to 17.8% in adoles-cents [3]. One engages in NSSI to express one's distress or to obtain a desired outcome for secondary gain [4]. Meanwhile, one may be at greater risk of self-harm from psychotic symptoms of underlying mental illness including auditory hallucination, thought insertion and delusion [5]. Such self-harm is an example of self-destructive behavior from psychosis [6]. Meltzer [7] reported that approximately 50% of people with schizophrenia experience self-injury. Additionally, common risk factors associated with self-injurious behaviors include major depressive disorder with psychotic features and manic episode of bipolar I disorder [8]. Although there are various psychological drivers of self-destruction, most forms result in cutaneous wounds. These wounds are often coupled with impaired wound healing and risk of infection because the underlying causes of self-mutilation are not easily corrected.
In this article, we share our experience of two cases with chronic wounds in the lower extremities following multiple episodes of self-harm due to different psychiatric issues. Furthermore, we highlight important aspects in treating the consequences of self-harm, proposing a systematic approach for successful wound management.
This study received an exemption from the Institutional review Board of St. Vincent's Hospital (Exemption No. VIRB-2022-1408-0001). Written informed consent to publish photo-graphs and case details was obtained from the patients.
Case
Case 1
A 47-year-old female with a history of sarcoidosis but no psychiatric history presented with partial dehiscence on the right ankle after primary closure of a wound that was initially a simple laceration caused by a fall. The skin defect, measuring 2 cm in diameter, was covered with a split-thickness skin graft (Fig. 1A and B). After 4 months, she presented again with a new defect of 3.0×4.0 cm in the right lower leg from another fall. An attempt had been made to heal the wound in the outpatient clinic (Fig. 1C and D). Despite the patient's denial, the medical care team strongly suspected that she had been reopening the wound because the previous dressing materials were always missing at every visit. After admission, a skin graft was placed over the defect which had been enlarged to 3.5×5.0 cm. Although the medical team suspected NSSI, the patient insisted that the wound was caused by accident instead of self-harm and refused to see a psychiatrist. Thereafter, she had been in and out of the hospital eight times due to repeated events (Fig. 2). This patient, a single woman living alone, showed an abnor-mal, strong attachment to one attending male physician and desired to remain hospitalized even when it was unnecessary. After 13 months, she harmed herself with a nail clipper; the wound gradually became infected and increased in size and depth due to repetitive wound picking. The 3.5×4.5 cm defect with muscle exposure was first covered with a rotational fasciocutaneous flap but was re-injured soon after (Fig. 1E and F). The anterior compartment of the lower leg was exposed and an infection had set in over the wound base (Fig. 1G). While performing serial debridement with a vacuum dressing, con-siderable time was spent building a good patient-physician re-lationship, encouraging patient engagement and consultation with a psychiatrist.
Fig. 1.
Progress photos of case 1. (A) A 2-cm round-shaped defect after surgical debridement. (B) Split-thickness skin graft coverage was done. (C) A 3×4 cm skin defect with exposure of the tendon was newly developed. (D) Wound contraction and epithelization in progress. (E) A 3.5×4.5 cm defect with muscle exposure was observed. (F) Rotational fasciocutaneous flap coverage with skin graft was performed. (G) Graft loss with chronic infection was noted. (H) An anterolateral thigh free flap was conducted. (I) Appearance at 5 months after surgery.
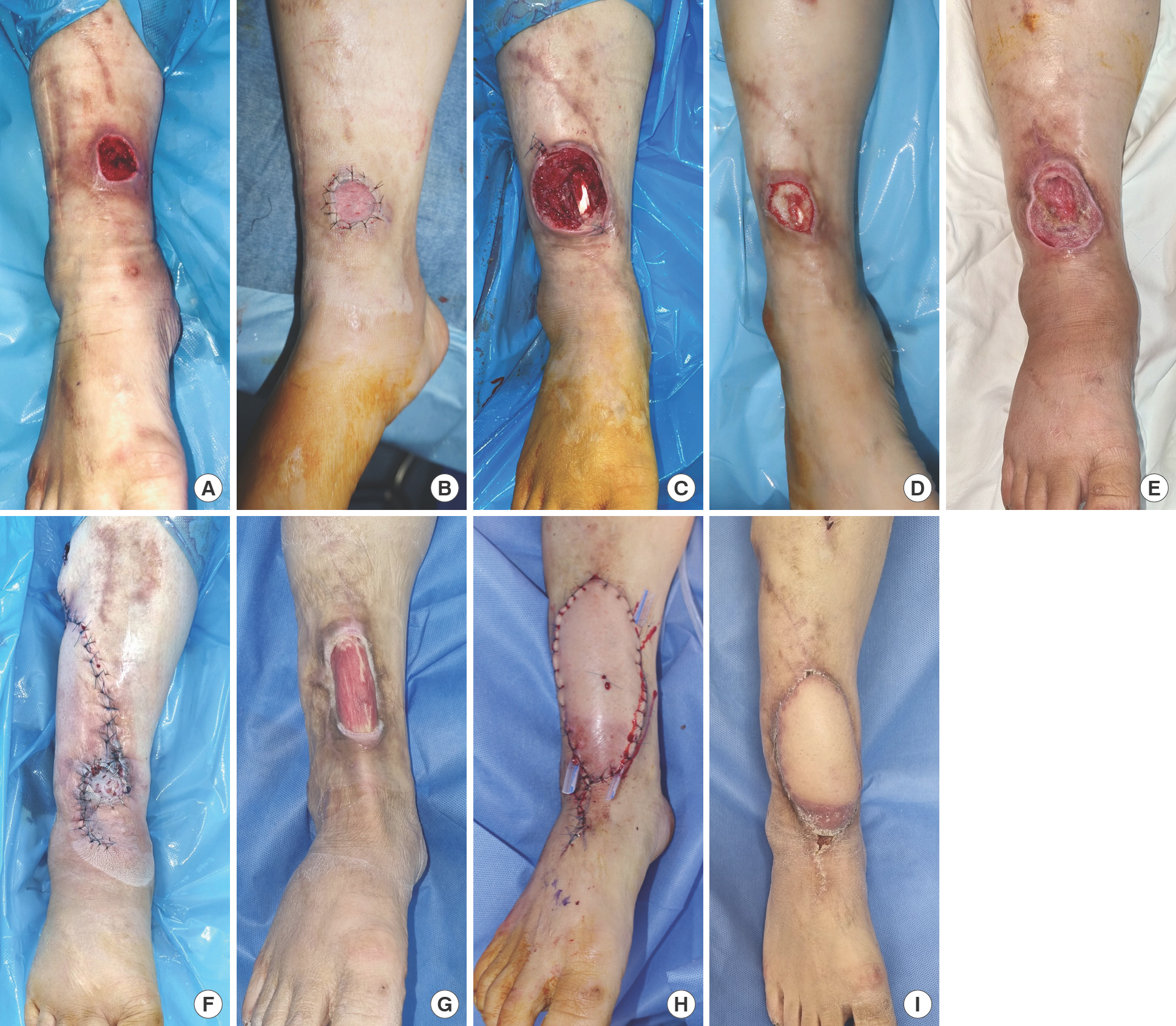
Fig. 2.
A timeline showing changes in the patient's wound condition. Orange line indicates the size of defect. Note that the wound score is inversely proportional to the defect size. Adm, admission; STSG, split-thickness skin graft. a) According to the Strauss Wound Scoring System, wound assessment was based on wound base appearance, size, depth, bioburden, and perfusion. Each characteris-tic was graded on a scale from 0 to 2 with a higher score corresponding to a healthier wound.

Under psychiatric consultation, the patient was diagnosed with bipolar disorder type I and comorbid panic disorder. The psychiatric treatment based on both cognitive behavioral therapy and medications such as antidepressants, anxiolytics, sed-atives, and antipsychotics, began in an outpatient setting. As continuous interdisciplinary care was offered, the patient began to understand that her anxiety and sense of emptiness would not be fundamentally resolved by self-mutilation. The patient stopped harming herself and became more cooperative with wound management along with medical and behavioral therapy for 6 consecutive months, and agreed to undergo free flap reconstruction knowing that another surgical procedure was not possible in the case of recurrence. In February 2022, the defect was covered using an anterolateral thigh free flap which was bulkier than necessary (Fig. 1H). To motivate the patient, the physicians told her that debulking surgery would be performed when the lesion was maintained for several months without injury. However, the patient consistently raked out the recipient vessel exploration scar on the foot dorsum and also made a small new wound on the opposite lower leg (Fig. 1I). Fortunately, there were no more attempts to make more wounds in the free flap skin territory.
Case 2
A 67-year-old man was admitted with a self-inflicted wound on the dorsum of his left foot. The patient had a history of dia-betes and a psychiatric diagnosis of schizophrenia. A skin graft was applied to a 2.0×2.0 cm defect (Fig. 3A and B). During follow-ups, the graft site healed without complications, but a small blister formed adjacent to the old wound due to adhesive plasters. The patient's wife was educated in how to care for the wound with hydrocolloids at home. However, after a month, the wound developed into a 3.0×7.0 cm subdermal fat layer defect (Fig. 3C). According to the patient's wife, she had dis-covered him picking his own skin many times when left alone. While the defect was completely closed with a split-thickness skin graft, graft loss was observed along with another superficial injury soon after. Signs of infection, such as swelling and erythema, were also observed (Fig. 3D and E). The patient's psychotic symptoms worsened simultaneously; he was in-creasingly talking to himself and showing impulsive behavior. After admission, wound management entailed the following: serial surgical debridement, daily dressing change, wound swab cultures, and appropriate systemic antibiotics under a microbiologist's advice. A referral to and visit with a psychiatrist yielded report of recent command hallucinations for self-harm. The consulting psychiatrist recommended an increase in antipsychotics dosage, resulting in favorable treatment re-sponse. Because longer hospital stays and repetitive surgical intervention heightened the patient's tension and anxiety, he was dismissed prematurely and secondary healing was at-tempted by providing a home-care dressing package (Fig. 3F). Currently, the patient remains under outpatient follow-up only when necessary while his wife is responsible for primary wound care.
Fig. 3.
Progress photos of case 2. (A) Initial skin defect of 2×2 cm with skin necrosis. (B) Split-thickness skin graft coverage was done. (C) While the initial wound was completely healed by skin graft, a new wound appeared proximally. (D, E) After a month, another wound was newly developed on the lateral side with signs of infection. (F) The most recent photograph showing multiple superficial skin defects, without signs of infection.

Discussion
There has been a global increase of patients who deliberately cause skin and soft tissue injury. In fact, recent statistics showed that one in ten people carry out some form of self-harm in their lifetime [1]. As psychological triggers differ between NSSI and self-destructive behavior that is due to psychosis, the characteristics of associated wounds also show different patterns. While the former presents as minor tissue damage such as simple lacerations or superficial defects, the latter is relatively more severe and sometimes fatal such as in cases of complicated lacerations or major self-mutilation [5,6]. Among the various types of self-manipulation, skin/wound picking and cutting are the two most common methods. Self-injurers often mutilate themselves in locations that are accessi-ble but easily hidden such as arms, legs, and the front of the body. There is limited data suggesting that choice of injury site is meaningful for sufferers [9]. It is estimated that 15%–16% of all self-harm presentations were due to repeat acts within a year, because underlying causes are not corrected easily [10]. The repetitive nature of self-harm usually induces the undesir-able progression of wounds from acute to chronic [3]. Con-ventional treatment including negative pressure wound therapy and reconstructive surgery is not necessarily a solution but rather creates a vicious cycle in which new wounds can devel-op. Therefore, understanding the psychology of self-harm and self-injury is crucial for surgeons to devise a differentiated, in-dividual therapeutic approach to treat cutaneous wounds caused by self-mutilating behaviors.
In this paper, case 1 represents NSSI, while case 2 represents self-destructive behavior arising from psychosis. NSSI has been linked to low self-esteem, which reflects one's negative beliefs of inferiority, worthlessness, and a sense of not belonging, triggering acute emotional distress that requires an outlet. Self-destruction is positively reinforced through feelings of relief and decreased tension. Additionally, one might exploit self-harm as a means of asking for help and achieving secondary gain [10]. Meanwhile, self-injurious acts due to psychosis have different characteristics. Although the mechanisms remain unclear, psychotic experiences stimulate self-mutilation via symptoms such as delusion and command hallucinations (i.e., voices directing one toward self-harm) [11]. We share our general principles for treating patients who harm themselves, not only for wound management but also for correction of different psychological drivers.
The first step is recognizing that the cause of wounds may be self-harm. It is difficult to identify self-harm because people who hurt themselves usually try to hide their injuries and scars. Clues that may imply self-mutilation include historical inconsistencies, incongruity between wounds and explanations, and repeated injury [3]. In case 1, self-harm was easily suspected because the wound showed poor correlation with the stated trauma mechanisms and also because the patient had been touching the wound repetitively. In case 2, the patient's family provided reliable information. Once self-injury is suspected, it is important to take a comprehensive history of psychiatric and medical conditions while also taking a detailed wound assessment including mechanism, size, depth, location, amount of exudate, and infection signs.
Second, wound management for self-inflicted wounds is generally the same as for other wounds, but it is particularly important to assess infection risk [12]. Because self-harm wounds are associated with chronic infection, treatment pro-tocols should include anti-bacterial dressings, serial surgical debridement, wound culture, proper systemic antibiotics, and pathologic confirmation, when possible. It should also be a priority to give clear explanations about treatment plans and invite patients to partake in the decision-making process be-forehand. This will help establish a good therapeutic relation-ship, resulting in improved patient compliance. Additionally, elastic bandages or tubular retentions should not be used if patients seem psychologically unstable because these bandages can be tools for suicide.
Third, referral to a psychiatrist is strongly indicated for patients who deliberately harm themselves. If a patient refuses psychiatric intervention as shown in case 1, attending physicians have the responsibility to emphasize the importance of such treatment. Communication and empathic listening can not only encourage emotional relief but also promote the patient's compliance with subsequent treatment. As described in case 2, those who injure themselves as a result of psychotic episodes are unlikely to repeat such self-harm once their underlying psychotic diseases are controlled by psychiatric intervention. Appropriate psychiatric treatment and adjunctive medi-cation (or escalation/switching) may be essential to protect patients from self-mutilation. Regardless of the psychiatric triggers, a stable clinical course of underlying mental illness is key to wound healing.
Finally, a self-care “rescue pack” can provide early patient-led intervention, by not only preventing cutaneous wound aggravation, but also by empowering patients to sustain their safety [8]. Rescue packs may contain gloves, dressing materials, and a wound-care leaflet that enables patients or guardians to effectively manage wounds by themselves. Early intervention with usage of such rescue packs is beneficial because it reduces repetitive hospital care and patient reliance on clinicians while reassuring them that they possess ownership of their care [13].
This article elaborates special insights associated with wound management in the light of different psychological drivers to further propose general guidelines for treatment of patients who deliberately harm themselves. The first thing that physicians must be aware of is that such wounds are difficult and sometimes even impossible to treat. Focusing merely on wound healing may lead to wound aggravation rather than re-covery. Additional tissue-damaging surgical treatment can increase the risk of wound manipulation and resulting complications by triggering a desire to inflict self-harm in a new location. We highlight the need for comprehensive history taking, wound assessment, early diagnosis, and timely intervention with psychiatric referral. Patient self-care using a rescue pack is helpful for ensuring active participation. Finally, psychoso-cial and emotional support with a non-judgmental attitude can promote a caring environment for patients to feel safe and respected, hopefully preventing further self-harm.















