Introduction
The human ankle joint maintains stability in a mortise and tenon structure. However, because the soft tissue around the joint is thin, the structures that maintain joint stability, including the ligaments and bone, are more vulnerable to traumatic injury. Here, we present a successful case of covering a severe soft tissue defect and bony structure destruction around the ankle resulting from a flame burn. The procedure enabled ambulation without complications in a patient who had been recommended for amputation at another hospital. The study was approved by the Institutional Review Board of Kangdong Sacred Heart Hospital (IRB No. 2019-11-008) and was conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from the patient for publication of his data.
Case
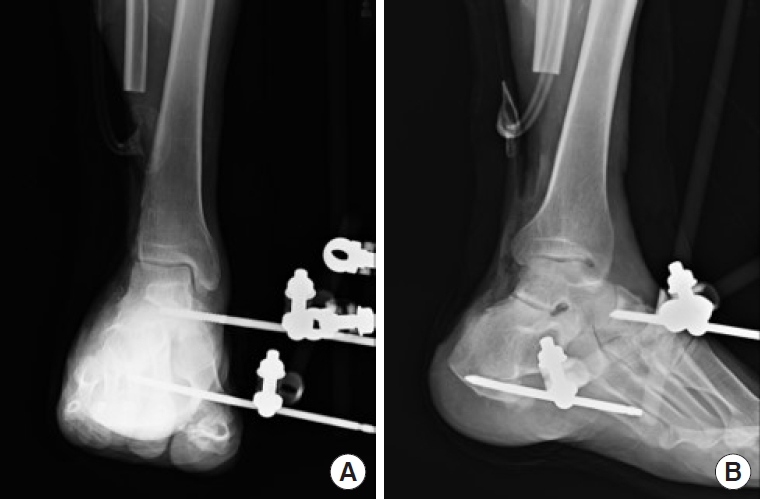
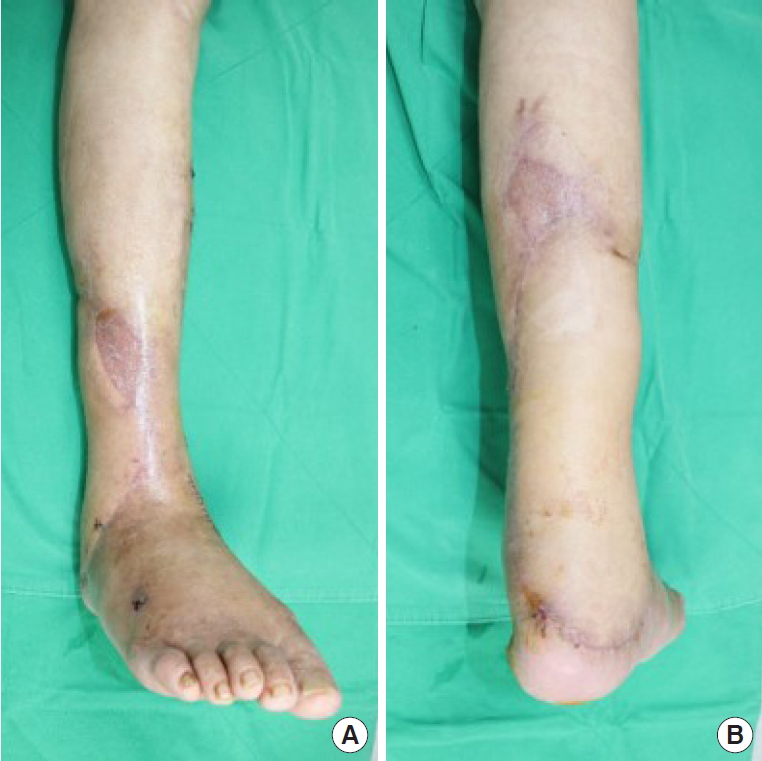
A 72-year-old man without underlying diseases lost consciousness due to inhalation of charcoal smoke and sustained a deep flame burn injury on his right posterior lower leg. He had been treated for the acute phase in a burn clinic and was referred to our institution for further management. The patient had a severe soft tissue defect from the midpoint of the calf to the posterior side of the ankle joint (25 cm in length, 15 cm in diameter) (Fig. 1). Necrosis occurred in the fibula, talus, and calcaneal bone that comprised the ankle joint, and the surrounding joint capsule and ligaments were also injured. Due to the extensive injury to the bony structures of the ankle joint and osteomyelitis, amputation had been considered. Because early ambulation is important to reduce complications that may occur after lower leg injuries, in severe injuries it is recommended to perform amputation as soon as possible and then to enable early ambulation with a prosthesis. However, patients generally find amputation unacceptable and may suffer psychologically after the operation. Here, the patient also showed a strong fear of amputation and expressed a desire to salvage the limb. Therefore, first we removed the distal half of the fibula, including the lateral malleolus and a part of the talus and calcaneal bone and applied an external fixator (EF) to fix the bony frame (Fig. 2). Then, we performed serial debridement to remove soft tissues showing necrotic change and administered intravenous antibiotics and negative-pressure wound therapy to clean the wound bed (Fig. 3).
Thereafter, we covered the soft tissue defect using an anterolateral thigh free flap and skin graft and temporarily fixed the ankle with an EF. Forty days after surgery, when the flap and skin graft had taken up well, we removed the EF in collaboration with the orthopedic department and fixed the ankle joint using tibiotalocalcaneal (TTC) intramedullary nailing perpendicular to the ground after passing through the calcaneal bone, talus, and tibia in the retrograde direction, along with ankle fusion and Chopart joint fusion to create horizontal stability (Figs. 4, 5). The patient began ambulation rehabilitation from 1 month after surgery and recovered weight-bearing and self-ambulation function within 1 month of commencing rehabilitation. One year after surgery, successful union was achieved between the ankle and Chopart joint; however, the subtalar joint showed no union (Fig. 6). Despite the fact that his gait was altered from that before surgery, the patient was adjusting well to daily life. Though he experienced a slight inconvenience in walking, his daily activities did not require too much movement, and the patient was satisfied with the surgery.
Discussion
In this report, we present a case of limb salvage with a relatively intact tibia and calcaneus bone structure in a patient with severe ankle damage. Determining the appropriate reconstruction method is challenging in patients with muscle and bone injuries. Although restoring preoperative function by reconstructing the pre-injury anatomical structures is ideal, devising an appropriate surgical plan in consideration of patient’s condition is crucial. In particular, lower limb injuries in older patients may reduce mobility, because a prolonged bed-rest results in reduced muscle tone. In the same way, preexisting morbidities may also be exacerbated, in turn further hindering mobility. Patients who are not independently mobile are at an elevated risk of complications, such as pressure sores, pneumonia, and deep vein thrombosis, and their mortality is increased from these conditions. Treatment that enables weight-bearing as rapidly as possible following surgery leads to better prognosis in older patients [1,2]. Therefore, if there is severe soft tissue damage, early amputation can be performed in order to shorten the time required until the patient is bearing weight with the prosthesis. However, amputation should be performed with caution, and salvaging the limb should be prioritized in cases where success is likely, particularly considering the postoperative psychological distress an amputation may cause.
The ankle joint maintains stability due to the shape of the talus and its compact placement between the tibia and fibula. The talus is located between the medial and lateral malleoli. The joint capsule, ligaments, muscle, and tendon connect them to maintain ankle joint stability [3]. Although this complex structure gives the ankle joint a wide range of motion, the thin soft tissue surrounding it makes it vulnerable to trauma. The patient in our case had half of the fibula injured, including the lateral malleolus, which damaged the fundamental bony structure of the ankle joint; therefore, amputation had to be considered. However, with amputation, weight bearing is generally started 3 months later; hence, we were concerned that the relatively delayed rehabilitation would decrease mobility and lead to complications. We, therefore, decided first to perform serial debridement and then salvage the limb using ankle fusion, because the tibia, talus, and calcaneal bone were relatively intact.
TTC intramedullary nailing is a fixation technique in which the calcaneus, tibia, and talus are vertically penetrated with a single piece of hardware, and stability of the joint can be attained by fixating the subtalar and tibiotalar joint movement. TTC intramedullary nailing is used as a successful salvage procedure in the presence of a severe injury or deformity of the ankle joint and hindfoot [4,5]. According to Al-Nammari et al. [1] and Jonas et al. [2], older patients can reach their preoperative functional level by 6 months after TTC intramedullary nailing, as they have a relatively lower functional demand [6-9]. Our patient started weight-bearing ambulation 1 month following ankle arthrodesis and reached his preoperative functional level without complications by 1-year follow-up. Although his gait altered from that prior to surgery, he did not have any discomfort in his daily activity.
A number of factors must be considered when planning reconstruction in a patient with severe soft tissue defect from a burn injury. As the field of plastic surgery directs much attention to soft tissue coverage, in most cases, surgeons focus on which flap to use to obtain coverage. However, in patients with severe defects including the joint, surgical planning should take into consideration the patient’s ability to resume their normal activity and also the incidence of potential complications.