Post-laparoscopy Epidermal Inclusion Cyst of Umbilicus
Article information
Abstract
Background
Epidermal inclusion cysts can develop in the umbilicus following trauma or surgery. In this study, we aim to report cases of epidermal inclusion cysts occurring at the umbilicus in patients with a history of previous laparoscopic surgery.
Methods
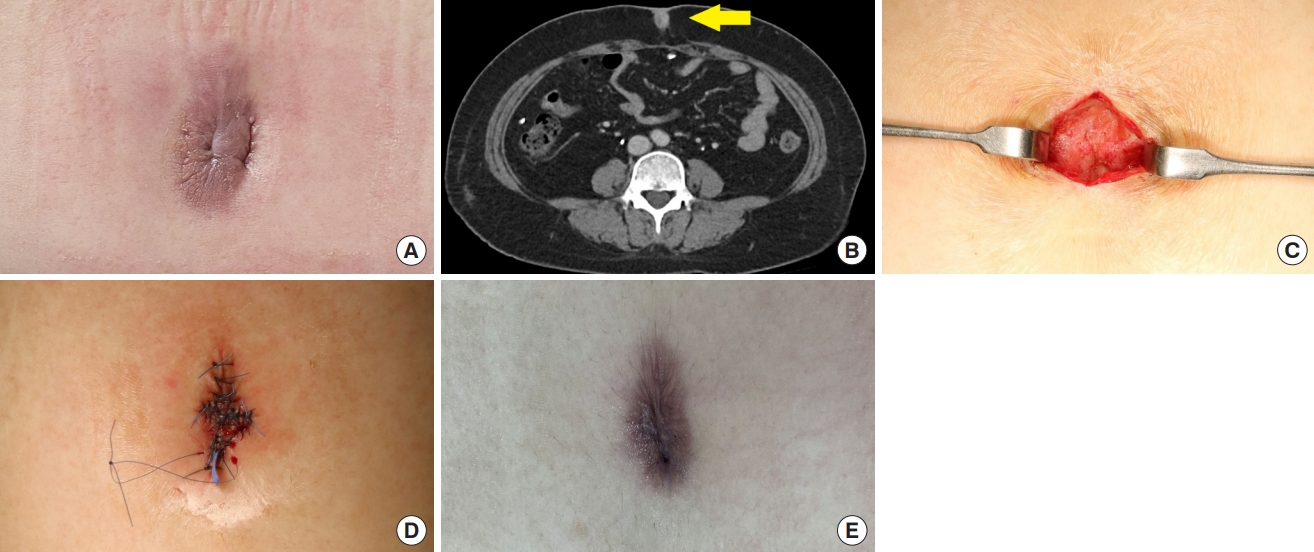
A retrospective study was conducted between January 2020 and May 2023 based on the medical records of patients who developed epidermal inclusion cysts in the umbilicus following laparoscopic surgery. Information regarding age, sex, symptoms, type of previous surgery, time elapsed from previous surgery to mass discovery, and postoperative complications was collected from a total of 15 patients.
Results
Out of the 15 patients, 13 were female (86.7%) and two were male (13.3%). Symptoms such as discharge, redness, and tenderness were present in 12 patients (80.0%). Obstetric and gynecologic laparoscopic surgeries were performed on 10 patients (66.7%), whereas general surgical laparoscopic surgeries were performed on five patients (33.3%). The mean time from laparoscopic surgery to discovery of the umbilical mass was 43.5 months. Wound dehiscence occurred in one patient (6.7%) and seroma developed in another patient (6.7%) out of 15 patients.
Conclusion
Achieving an ideal shape of the umbilicus after removal of epidermal inclusion cysts that occur at the umbilicus following laparoscopic procedures requires significant effort. Through this study, we aim to remind laparoscopic surgeons that epidermal inclusion cysts can develop at the umbilicus through laparoscopic interventions and thereby emphasize the importance of proper wound management.
Introduction
Epidermoid cysts are benign cutaneous tumors that originate from the follicular infundibulum. They form cysts by accumulating keratin within the epithelial lining [1]. Epidermoid cysts can manifest anywhere in the body but are most frequently found in the face, neck, chest, and upper back. They typically present as nodules within the dermal or subcutaneous layer [2]. While they can develop spontaneously, they may also arise as a consequence of implantation of the epithelium following surgery or trauma, leading to the formation of an epidermal inclusion cyst [1].
The umbilicus, which is formed at birth, serves as the connection between the fetus and the umbilical cord, typically appearing as a depressed scar [3]. It plays a crucial role in the abdominal contour and any abnormality or absence of the umbilicus can cause discomfort for patients, affecting the overall aesthetic appearance of the abdomen [4]. Given that the umbilicus is commonly used as an incision site in laparoscopic surgery, proper perioperative and postoperative care is essential to preserve its characteristic concave shape and prevent infections [5]. This study presents the findings of 15 patients diagnosed with epidermal inclusion cysts in the umbilicus who had previously undergone laparoscopic surgery. By raising awareness of the possibility of epidermal inclusion cysts occurring in the umbilicus among patients undergoing laparoscopic procedures across various departments, we aimed to enhance the understanding and management of this condition.
Methods
After obtaining approval from the Institutional Review Board of Eulji University Hospital (EMC 2023-06-009), a retrospective study was conducted based on the medical records of patients who visited the department of plastic and reconstructive surgery of our hospital between January 2020 and May 2023 with a chief complaint of umbilical mass. The inclusion criteria were as follows: (1) patients of all ages and both sexes; (2) patients with an umbilical mass; (3) patients who had previous laparoscopic surgery through the umbilicus; and (4) patients diagnosed with epidermal cyst by histological analysis. The exclusion criteria were as follows: (1) patients whose postoperative diagnosis of umbilical mass was not identified as an epidermal cyst; and (2) patients lost to postoperative follow-up.
Data on patient age, sex, symptoms, type of previous surgery, time elapsed from the previous surgery to mass discovery, and complications were obtained from the medical records. The patients provided written consent for the use of their photographs.
Umbilicus reconstruction technique
An excision was performed by marking along the margin of the umbilical mass and surrounding laparoscopic scar and skin. Following excision, the size of the defect was assessed, and both the horizontal and vertical dimensions were measured to determine the direction of local flap advancement, assumed to be in the direction of the shorter axis. Subcutaneous undermining was conducted to reduce tension. Irrigation was performed with a mixture of normal saline and antibiotics. Subsequently, an anchoring suture was placed using #3-0 polydioxanone (PDS) to secure the dermis to the linea alba or scar tissues. The subcutaneous layer was closed using a simple suture technique with #4-0 or 5-0 PDS. Skin was closed with #4-0 or 5-0 nylon using a simple suture method. After applying sodium fusidate ointment, fluff gauze was used to mold the concave shape of the umbilicus by compression, followed by application of an elastic abdominal binder. The nylon sutures were removed after 2 weeks. Subsequently, compressive dressings and elastic abdominal binders were utilized for an additional 2 to 4 weeks to shape the umbilicus.
Results
Among 19 patients who presented with a mass of the umbilicus following a past history of laparoscopic surgery, four patients who were not diagnosed with an epidermal inclusion cyst were excluded. The final analysis included 15 patients, consisting of two males (13.3%) and 13 females (86.7%). The age of the patients ranged from 26 to 75 years, with an mean age of 50.9 years. Among the patients, 10 (66.7%) had undergone obstetric and gynecologic laparoscopic surgeries such as myomectomy, hysterectomy, and salpingo-oophorectomy, whereas five (33.3%) had undergone general surgical laparoscopic procedures such as cholecystectomy and gastric band surgery. Of the 15 patients, discharge was reported in 12 patients (80%), redness in two patients (13.3%), and tenderness in three patients (20%). The size of the umbilical masses varied among the patients. One patient (6.7%) had a long radius of less than 1 cm, two patients (13.3%) had a long radius from 1 cm to less than 2 cm, three patients (20.0%) had a long radius from 2 cm to less than 3 cm, four patients (26.7%) had a long radius from 3 cm to less than 4 cm, four patients (26.7%) had a long radius from 4 cm to less than 5 cm, and one patient (6.7%) had a long radius of 5 cm or more. The mean time from laparoscopic surgery to the discovery of an umbilical mass was 43.5 months. One patient (6.7%) experienced wound dehiscence, which was successfully managed with outpatient wound repair. In one patient (6.7%), a small amount of seroma persisted at the surgical site for 4 weeks; however, it was successfully managed through conservative treatment on an outpatient basis (Table 1). The postoperative outcomes were assessed subjectively by the surgeon through outpatient follow-up. Among the 15 patients, four (26.7%) exhibited relatively similar shapes to normal umbilicus, while two (13.3%) displayed excessive horizontal scarring. The remaining nine patients (60.0%) experienced some degree of umbilical blunting, resulting in decreased depth or asymmetric deformity.
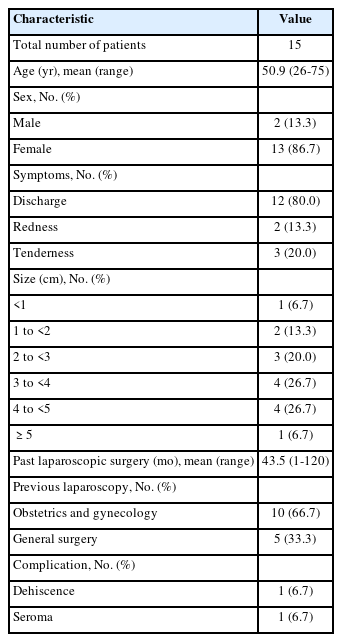
Case 1
A 63-year-old woman presented to the hospital with a mass accompanied by white discharge in the umbilical area that had developed approximately 5 years prior. The patient had undergone laparoscopic myomectomy at the obstetrics and gynecology department 10 years before her visit. Physical examination did not reveal tenderness or peripheral redness, whereas computed tomography (CT) scan indicated the presence of an inflamed umbilical mass. The patient underwent umbilical reconstruction following the excision of the mass measuring approximately 5.0×2.5 cm, along with all surrounding scar tissue. Because of the large defect after excision, it was necessary to excise additional normal tissues horizontally to mold a more natural-looking shape of the umbilicus. A postoperative histological analysis confirmed the mass to be an epidermal cyst. Four months after the procedure, concaveness was maintained, but an inevitable horizontal scar was present because of the additional excision of normal tissues (Fig. 1).
A case of a 63-year-old woman. (A) Preoperative photograph of the umbilical mass. (B) Preoperative computed tomography of the umbilical mass (yellow arrow). (C) Intraoperative photograph of umbilical area after excision of the mass. (D) Photograph after wound closure. (E) Postoperative photograph at 4 months.
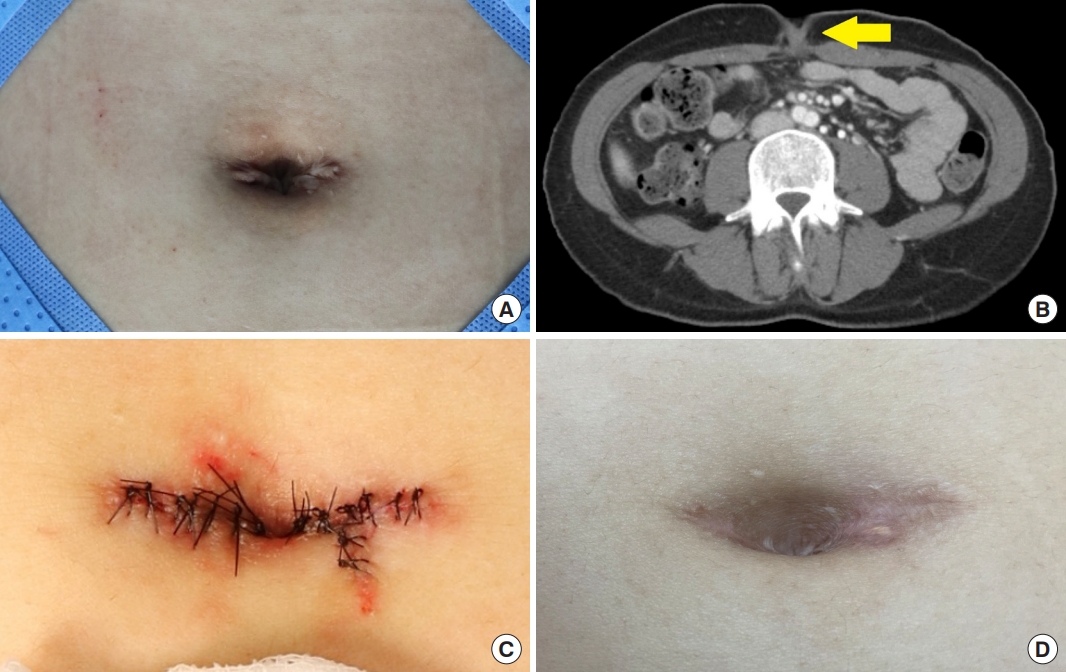
Case 2
A 40-year-old female patient visited the hospital due to a mass in the umbilical region, which had emerged along with discharge 2 weeks earlier. The patient had undergone laparoscopic gastric band surgery 10 years prior. Tenderness or redness accompanied the lesion, and a CT scan indicated the presence of an inflamed mass in the umbilicus. The patient underwent removal of the umbilical mass measuring approximately 2.0×1.5 cm. Postoperative histological analysis confirmed the presence of an epidermal cyst. Two months after surgery, the depth of the umbilicus became shallower compared to immediately after the surgery (Fig. 2).
A case of a 40-year-old woman. (A) Preoperative photograph of the umbilical mass. (B) Preoperative computed tomography of the umbilical mass (yellow arrow). (C) Intraoperative photograph of umbilical area after excision of the mass. (D) Photograph after wound closure. (E) Postoperative photograph at 2 months.
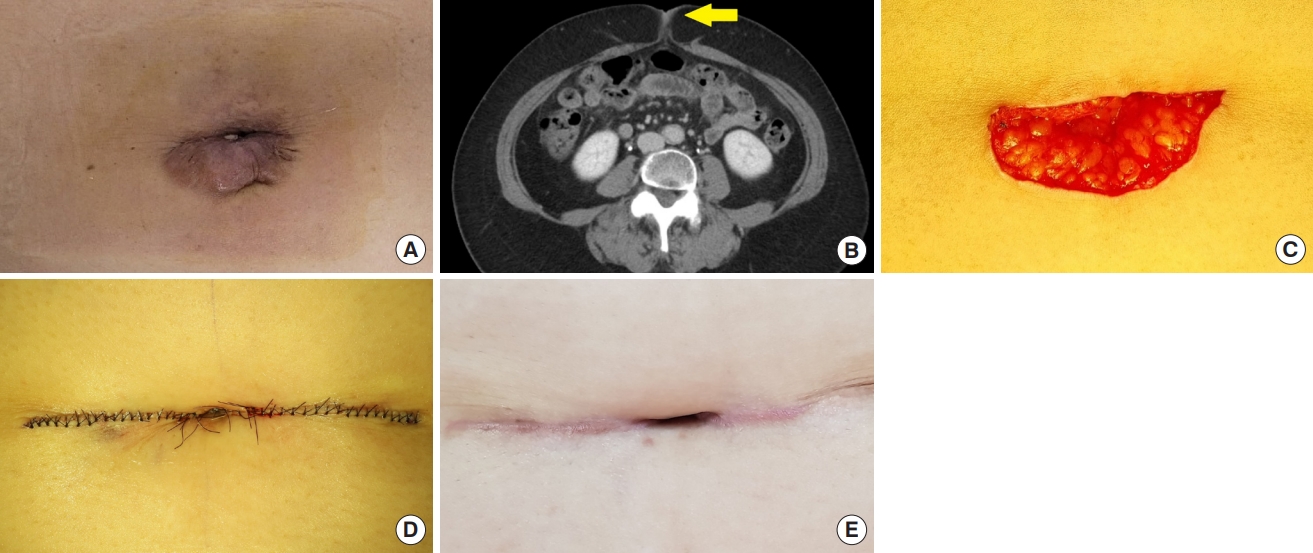
Case 3
A 33-year-old woman presented to the hospital with a mass in the umbilical area that had appeared approximately 4 years earlier, accompanied by tenderness and discharge. The patient had a history of laparoscopic ovarian cystectomy 1 year before her mass appeared. In the physical examination, there were no signs suggestive of inflammation such as redness or discharge, while a CT scan indicated the presence of an inflamed umbilical mass. The mass in the umbilicus, along with the surrounding scar tissue, was completely excised, and the size of the mass was measured to be approximately 2.0×0.5 cm. The mass was confirmed as an epidermal cyst by postoperative histological analysis. Six months after surgery, while there was slight asymmetry in the shape of the umbilicus, it generally maintained a natural appearance (Fig. 3).
Discussion
Epidermoid cysts are a type of cutaneous cyst characterized by a lining composed of epithelial cells. While they can occur spontaneously, they can also manifest as epidermal inclusion cysts, wherein epidermal cells become embedded inside. These cysts typically develop after trauma or surgery. Histologically, they are surrounded by stratified squamous epithelial cells containing keratin in their lumen [1]. Epidermoid cysts are generally benign tumors that are treated through surgical excision. In this study, we analyzed 15 cases of epidermal inclusion cysts that were removed from the umbilicus and reconstructed in patients with a history of previous laparoscopic surgery and robot-assisted laparoscopic surgery.
Among the total of 15 patients in our study, 12 patients experienced symptoms such as discharge, tenderness, or redness. Differential diagnosis of the epidermal cyst was essential based on the clinical features of the patients, and the presence of a cystic lesion in the umbilical area was confirmed through CT scan. The umbilicus is regarded as a scar with a distinct concave structure. Structurally, it contributes to defining the contours of the abdomen and medial abdominal sulcus [3]. Because the cosmetic aspect depends on the appropriate size and shape, the absence or abnormal appearance of the umbilicus can lead to psychological and social discomfort in patients, hence the importance of reconstruction [3,4]. Most patients presented with an irregular shape of the umbilicus with a loss of concavity at the time of their visit. Our efforts focused not only on the complete removal of the mass but also on molding the concave contour of the umbilicus.
The time interval between laparoscopic surgery and discovery of the umbilical mass varied from 1 to 120 months, with an mean of 43.5 months. This underscores the importance of regular outpatient follow-ups, even in the absence of symptoms, following laparoscopic surgery. Among the patients, two (13.3%) experienced complications of dehiscence or seroma after removal of the cyst. However, these complications were successfully addressed through outpatient procedure, without the need for hospitalization or further surgery. The size distribution of the cysts varied, ranging from less than 1 cm to over 5 cm, with the majority between 3 and 5 cm.
Epidermal cysts are often found within the vicinity of compromised or unhealthy tissues. Moreover, when patients present with an umbilical mass, the internal size could be larger size than visible externally, and in some cases the mass might be ruptured. Therefore, more extensive excision might be necessary, and reconstructing the umbilical shape could be challenging. Various methods for umbilical reconstruction have been reported [6], but in this study, the primary focus was initially on the complete excision of the epidermal cysts. We excised the entire mass along with the surrounding laparoscopic scar and skin. Subsequently, efforts were directed towards sustaining the concave shape of the umbilicus over an extended period. Firstly, subcutaneous undermining was done to create depth by anchoring sutures in the abdominal wall, and secondly, monofilament sutures were used to reduce the possibility of inflammation or infection. Additionally, to mold the concavity postoperatively, compressive dressing was maintained for 4 to 6 weeks, and the use of an elastic abdominal binder was continued to prevent early release of anchoring sutures caused by abdominal muscle contraction.
In case 1, where a cyst with a diameter of 5 cm was present, a horizontal incision had to be added after excision, resulting in inevitable scars on both sides of the umbilicus. In case 2, reduction in the concaveness of the umbilicus was observed 2 months after the procedure. In case 3, 6 months after surgery, the concave shape of the umbilicus was well-preserved; however, the shape was asymmetrical and appeared irregular. Among the 15 patients, while four patients (26.7%) maintained a relatively favorable umbilical shape, other patients experienced excessive scarring or, over time, a reduction in dimpling and an irregularity in the umbilical shape. Despite significant efforts, maintaining an aesthetically superior umbilical shape remains challenging. Therefore, this study emphasizes the significance of preventing the occurrence of epidermal inclusion cysts in the umbilicus. Additionally, considering that the mean time interval from laparoscopic surgery to the discovery of the mass was 43.5 months, we suggest the importance of early detection and treatment for patients who develop such cysts before removal and wound management become more challenging.
Laparoscopic surgery offers advantages including reduced wound-related complications and shorter recovery periods. In many cases, laparoscopic surgery involves the insertion of trocars through the umbilicus. In this study, the patients had no specific history related to the umbilicus other than their past history of laparoscopic surgery. Furthermore, cysts developed at the site of trocar insertion, and all patients with symptoms experienced them after laparoscopic surgery. We speculate that the characteristic shape of the umbilicus as a distinct anatomical concave structure in the human body contributed to the embedding of epithelial components during laparoscopic surgery. Therefore, we believe that laparoscopic surgery is highly likely to induce epidermal inclusion cysts in the umbilicus. Given these points, if epidermal inclusion cysts develop in the umbilicus after laparoscopic surgery, the advantages of the laparoscopic approach could be compromised. Furthermore, considering that the patients in this study discovered the cysts on mean 43.5 months after laparoscopic surgery, it suggests prolonged discomfort over an extended period. With the increasing adoption of robot-assisted laparoscopy in recent years, there has been a growing interest in laparoscopy in general. This study aims to inform surgeons about the potential occurrence of epidermal inclusion cysts in the umbilicus following laparoscopic surgery and emphasizes the need for careful wound management during and after surgery.
The occurrence of epidermal inclusion cysts after minimally invasive strategies has been reported in the literature. Liposuction is often utilized as a minimally invasive surgical technique. Bechara et al. [7] presented a case report of a 35-year-old female who developed multiple epidermal inclusion cysts in the axilla after liposuction. Similar reports have been additionally reported. Posthuma et al. [8] reported a case of a 49-year-old male who developed an epidermal inclusion cyst following minimally invasive surgery for a calcaneal fracture. These cases suggest that minimal invasive surgeries, because of their small incisions and frequent instrument-tissue interactions through these small incisions, can lead to easy implantation of epidermal cells. A case report also described a 44-year-old male who developed an epidermal inclusion cyst at the site of incision on the palm after receiving mini-open carpal tunnel release [9]. Considering these reports collectively, there could be an association between laparoscopy and epidermal inclusion cysts occurring at the umbilicus. Surgeons should take care during laparoscopy to prevent deep penetration of epithelium into underlying tissues when making incisions or inserting trocars. One potential approach could involve using film dressings to protect the incision margin before trocar insertion. Further research in this area is warranted.
While there have been a few case reports on epidermoid cysts in the umbilical area, this study is considered the first to investigate a large number of patients with epidermal inclusion cysts specifically occurring in the umbilicus after laparoscopic surgery. Prior to this study, there were less than 10 published articles discussing epidermal inclusion cysts in the umbilicus, and among them, cases arising after laparoscopic surgery through the umbilicus were even more rarely reported [10]. Andreadis et al. [11] reported the case of a 39-year-old woman with an epidermal inclusion cyst in the umbilicus following abdominoplasty. Lee and Yang [4] described a 49-year-old woman who underwent reconstruction using a three-point crossover technique for an umbilical epidermoid cyst that developed after laparoscopic uterine myomectomy, and Li and Robertson [10] reported on a 52-year-old woman who had an umbilical epidermal inclusion cyst after laparoscopic surgery for endometriosis.
Through this study, we aim to raise awareness among surgeons about the possibility of epidermal inclusion cysts in the umbilicus after laparoscopy and emphasize the importance of careful wound management through the umbilicus. Secondly, we intend to introduce a simple technique for umbilical reconstruction in patients who develop such post-laparoscopy epidermal inclusion cysts. The findings of this study could provide valuable insights to various laparoscopic surgeons and medical professionals treating patients with umbilical masses.
Notes
No potential conflict of interest relevant to this article was reported.