Demodicidosis of an Intertragic Notch of the Ear That Was Misdiagnosed as a Skin Tumor: A Case Report
Article information
Abstract
Demodex mite infestation has variable clinical manifestations including eruptions, erythema, pustules, facial hyperpigmentation, rosacea-like lesions, and perioral dermatitis. A 62-year-old man came with a 2-year history of a slowly enlarging, asymptomatic lesion in the intertragic notch of the left ear, and the findings from an ultrasound conducted by a radiologist suggested a benign skin tumor such as an epidermal or trichilemmal cyst. After total excision, histopathology of a section of the specimen showed multiple follicular infundibula containing Demodex folliculorum in the dermal layer, and the perifollicular tissue showed granulomatous change with lymphomononuclear inflammation. This article presents a rare clinical symptom of Demodex mites in the form of a tumor-like lesion on the face.
Introduction
Human demodicidosis (DD) is a skin disease of the pilosebaceous units that is caused by human Demodex, a well-known ectoparasitic mite that primarily affects the face and head [1-4]. Demodex mites are ectoparasites of humans that live in or near pilosebaceous units and feed on sebum as nourishment [5,6]. Demodex folliculorum and Demodex brevis are the two common types that infest humans. Such infestations are usually asymptomatic and have a pathogenic role only when the mites are present in high densities or when the individual has an immune imbalance [6]. Clinical manifestations include a group of eruptions characterized by variable degrees of spinulosus, erythema thema and pustules, facial hyperpigmentation, blepharitis, rosacea-like lesions, and perioral dermatitis usually accompanied by a burning or pruritic sensation [2,7]. This article introduces a case of DD infestation that manifested as a rare clinical symptom–in the form of a tumor-like lesion. The patient provided written informed consent for the publication and use of his images.
Case
A 62-year-old man presented with a 2-year history of a slowly enlarging, asymptomatic lesion in the intertragic notch of the left ear (Fig. 1). This patient had no specific medical history or immunosuppressive diseases, and only complained of the growing size of the lesion but not of discomfort such as itching or pain. On physical examination, a 1.5 cm dome-like solitary lesion that had an elastic yet hard texture resembling a skin tumor was found. Before deciding to surgically remove the tumor, ultrasound examination was done by a radiologist. The tumor was suspected to be a benign skin tumor similar to epidermal or trichilemmal cysts, and ultrasound revealed a 1.6×1.2×1.1 cm lobulated heterogeneous hypoechoic lesion without significant vascularity in the subcutaneous fat layer (Fig. 2). Under local anesthesia, an incision was made around the mass, and the dissection was deepened until the cartilage layer was reached. The tumor-like lesion in the intertragic notch of the left ear was completely excised. A full-thickness section of the skin was harvested from the left retro-auricular area and was used to cover the defect site with a tie-over dressing (Fig. 3). The excised lesion was sent to the pathology department and a permanent section of the specimen showed multiple follicular infundibula containing D. folliculorum in the dermal layer, and the perifollicular tissue showed lymphomononuclear inflammation (Fig. 4). At the 2-month postoperative follow-up, the recipient site was in good condition and the donor site was without complications. There was also no recurrence (Fig. 5).

Preoperative image of the ear. Asymptomatic tumor-like lesion in the intertragic notch of the left ear.
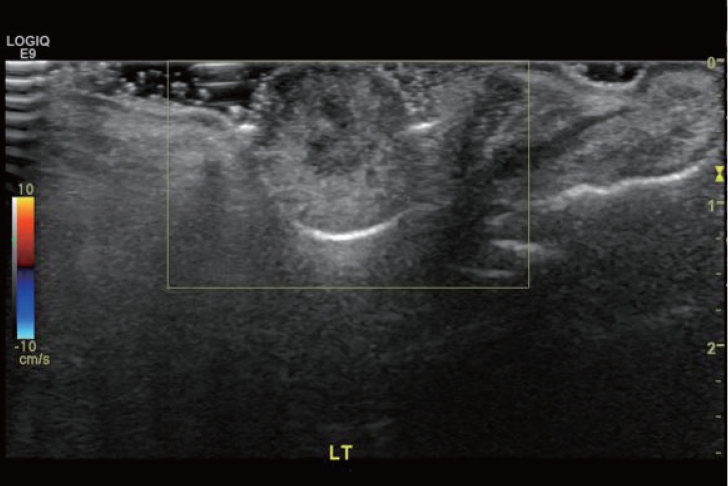
Preoperative findings from an ultrasound conducted by a radiologist. A 1.6×1.2×1.1 cm lobulated heterogeneous hypoechoic lesion without significant vascularity in the subcutaneous fat layer is suspected to be a benign skin tumor, such as an epidermal or trichilemmal cyst.
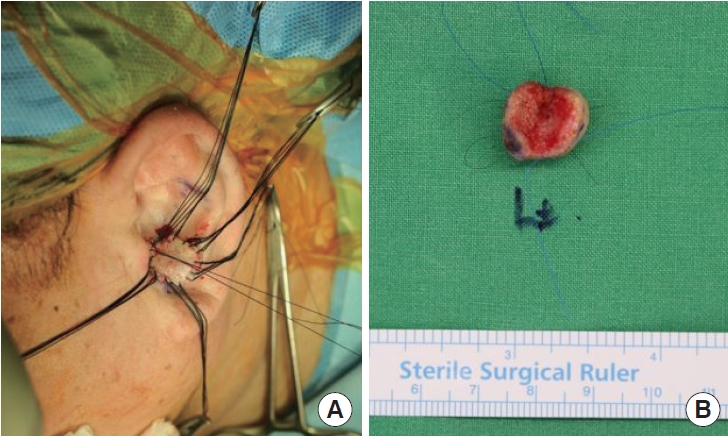
Intraoperative image. After excision, a full-thickness skin graft was performed (A) and the excised specimen (B).
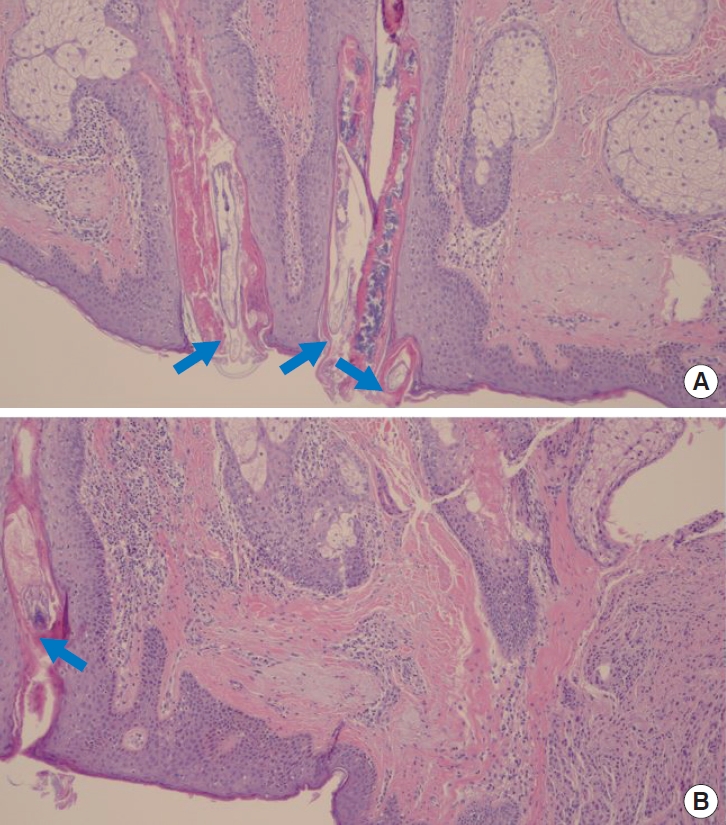
Pathologic findings showing Demodex-associated inflammatory granuloma. Demodex folliculorum (blue arrows) in the hair follicles (A). Lymphomononuclear inflammation around the perifollicular tissue (blue arrow) are seen (B). Hematoxylin and eosin staining, ×200.
Discussion
Human DD is caused by infestation of two types of Demodex mites, D. folliculorum and D. brevis. Although human demodicosis presents a wide range of clinical symptoms that mirror many different dermatoses, it is important to keep in mind the etiological role of this adaptable mite [6]. Commonly, various therapeutic regimens have been proposed to treat DD, including acaricides and adjuvants, such as systemic and topical metronidazole [2].
In this case, a healthy 62-year-old man presented to our department with a 2-year history of a slowly enlarging, asymptomatic lesion in the intertragic notch of the left ear. The pathologic findings of a permanent tissue section were consistent with granulomatous inflammation associated with D. folliculorum in the hair follicle. Microscopically, demodicosis has follicular and perifollicular chronic inflammation with follicular dilatation and dense homogenous eosinophilic reactions surrounding the mites. Granulomatous tissue reaction may also be present.
Previously published articles described this pathologic reaction as originating from the epithelioid histiocytes, beginning within the bone marrow as myeloid precursors that mature into monocytes, eventually entering peripheral circulation. In contrast to inactivated, reniform histiocytes with defined cell boundaries, the innate immune response provides the activated histiocytes their distinctive epithelioid look. After the acute phase, activated histiocytes remain and take over the chronic inflammatory response and subsequent tissue repair. In the chronic phase, wound repair and fibrosis could be continuously induced while maintaining the balance of inflammation and promoting phagocytosis. Therefore, chronic inflammation could form focal nodular lesions of granuloma and could be misdiagnosed as a nodule or benign tumor [8,9].
Previous articles were not sufficient to establish standardized therapeutic regimens for demodicosis in forms of tumors. Although a variety of treatment plans have been suggested for DD, including acaricides, as well as adjuvants including benzyl benzoate, salicylic acid, gamma benzene hexachloride, sublimed sulfur, and systemic and topical metronidazole, the best method of treatment is still up for debate [2,7]. In this case, our patient was successfully treated after total excision with no recurrence.
In conclusion, it is important to consider patient history when making the diagnosis, and to perform a preoperative evaluation skin and soft tissue mass through radiological examination. However, Demodex infestations with atypical clinical characteristics can be difficult to diagnose, even based on patient history and imaging examinations. This case has shown that Demodex mites can cause a rare type of clinical symptom in the form of a lesion that looks like a tumor. This suggests that chronic infections in healthy people that can look like tumors, such as parasitic, viral, or fungal infections, as well as those caused by Demodex, should also be thoroughly investigated by clinicians.
Notes
No potential conflict of interest relevant to this article was reported.

