A Case Report of Extensive Penile Inflammation from Dermofat Graft
Article information
Abstract
Dermofat grafting is one of the most commonly used procedures for soft tissue augmentation. It requires precise excision of the epidermal layer during harvesting; however, a residual epidermal layer is sometimes observed on the dermofat graft. Here, we describe a case of extensive penile inflammation caused by the residual epidermal layer of a dermofat graft. En bloc excision of the residual epidermal layer of the dermofat graft and Buck’s fascia enabled complete healing without sequelae.
Introduction
Since dermofat grafting was first used for penile augmentation in 1992, it has been established as one of the most classical procedures for augmentation purposes. With a relatively low fat absorption rate, the method shows high success rates for grafting [1-3]. Moreover, as an autologous graft, it demonstrates a lower risk of rejection. However, dermofat grafting has a potential risk of infection [1,2]. Several factors increase the possibility of dermofat graft infection, such as inappropriate antibiotic usage or damage to the graft during harvest. Among the latter, a residual epidermal layer caused by incomplete excision of the epidermis is a lesser-known but critical factor. In this report, we explore a case of widespread infection resulting from penile augmentation through dermofat grafting without precise de-epithelization. The study was approved by the Institutional Review Board of Hallym University Hospital (IRB No. 2022-03-0009). The patient provided written informed consent for the publication and use of his images.
Case
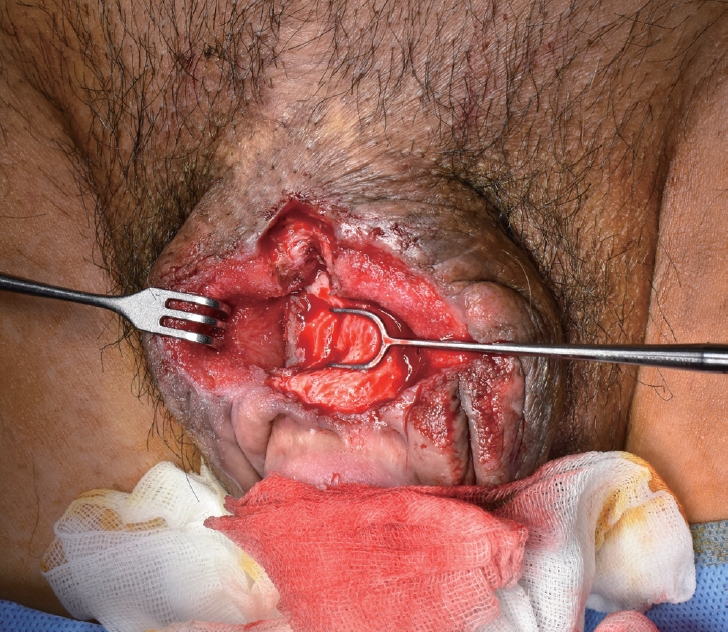
A 60-year-old man with extensive penile inflammation was referred to our department (Fig. 1). He stated that there was pus discharge and the pain and swelling had gradually aggravated. Symptoms arose spontaneously from 5 days before the patient’s first visit to our hospital without triggers such as trauma or coitus. He had undergone penile augmentation surgery with a dermofat graft from the right buttock area at a private clinic 17 years prior. Several attempts for debridement and closure of the wound performed at the urology department to care for the infected wound were unsuccessful. Laboratory tests taken after referral revealed C-reactive protein levels of 250 mg/L, and a and a fever of >38.0 °C was observed with tachycardia. These findings suggested that penile inflammation worsened the patient’s general condition which could lead to potentially life-threatening sepsis. After Enterobacter cloacae was observed from wound cultures, meropenem antibiotics were administered. Hemoglobin A1c had also significantly increased to 10.2%, indicating severe uncontrolled diabetes.

Initial clinical photography when the patient visited the urology department. Extensive penile inflammation is observed.
Even with aggressive debridement of inflamed tissue performed at our department, the wound was not clean enough to close (Fig. 2). We applied negative-pressure wound therapy (NPWT) for 3 weeks and tried a nanocrystalline silver antimicrobial barrier dressing (Acticoat, Smith & Nephew). However, the wound did not substantially improve and was still not sufficiently clean enough. As additional wound cultures yielded bacteria identical to the initial results, meropenem administration was maintained. To obtain a clean healthy wound, we decided to perform en bloc excision including normal tissue rather than merely debriding the inflamed tissue (Figs. 3, 4), after which the wound was completely closed immediately. Intraoperatively, a biopsy of the excised wound tissue was performed. Histological examination confirmed that the wound base tissue obtained from Buck’s fascia was covered with an inflamed epidermal layer indicating that some epidermal layer of the dermofat was grafted together, and epithelialization occurred in both the dermofat and Buck’s fascia (Fig. 5). This residual epidermal layer, along with the patient’s severe diabetes, was suspected to have caused extensive penile inflammation. The sutured site completely healed, without complications (Fig. 6). Antibiotics were maintained for 6 weeks before the patient was discharged. One year after the operation, there was no hypertrophic scarring or contracture of the penile shaft, and the patient was satisfied with the result (Fig. 7).

Histologic findings of the surgical specimen. Inflamed granulation tissue (arrowhead) with epidermal squamous cells (arrow) is observed (hematoxylin and eosin staining, ×100).

Postoperative clinical photography 14 days after the operation. The wound healed without complications.
Discussion
Dermofat grafting is commonly performed for soft tissue augmentation. It is used in various fields, including aesthetics, congenital anomalies, and deformities due to trauma or cancer [2]. Dermofat grafts include a full-thickness dermis and a subcutaneous fat layer. The thickness and number of fibroblasts in these layers differ according to the harvest method [4]. Harvest sites include the upper and lower buttocks, lower abdomen, lateral abdomen, and inner thigh [5]. During the surgical procedure, precise excision of the epidermis by a dermatome, shaving razor, or electrocautery is mandatory. Damage to the subcutaneous layer should be minimized during the surgical procedure to reduce the absorption rate. The absorption rate of dermofat grafts is 10% to 20%, which is much lower than that of fat injections [1,3,6]. Moreover, since dermofat graft is autologous, the possibility of rejection or foreign body reaction is low [1,2].
Dermofat grafts are also widely used for penile augmentation, because they can provide a smooth contour without irregularities and show a better fat graft survival rate than fat injections [7,8]. The harvested dermofat is placed in the pocket above Buck’s fascia. Enough space should be secured in this pocket to prevent graft necrosis and to increase the graft success rate. It is possible to prevent postoperative graft necrosis and increase the success rate by widening the space where the graft is to be placed using a penile stretcher or an external cutaneous expander as a preoperative adjuvant method to maximize the surgical outcome. According to the literature, penile girth and length can be increased by approximately 20% and 30%, respectively, after dermofat grafting [5,9].
Infection is one of the most common complications associated with the dermofat graft [1,2]. The penis is particularly one of the most vulnerable organs susceptible to infection. It is difficult to manage hygienically compared to other parts of the body and should also tolerate considerable physical fatigue. Therefore, dermofat grafts used for penile augmentation are more susceptible to infection. However, unlike the most common cases of dermofat graft inflammation, we presumed the reason for inflammation in this case to be the residual epidermal layer of dermofat and the patient’s poor general condition, which made the patient vulnerable to inflammation, compounded by aggravated local infection. The intraoperative biopsy revealed that the dermofat graft and Buck’s fascia were covered with an inflamed epidermal layer. Since the epidermal layer cannot be observed in normal Buck’s fascia, it is reasonable to assume that these epidermal layers were derived from the grafted dermofat. Squamous epithelial cells constituting the epidermis undergo mitosis and migration, causing re-epithelialization of the dermofat graft. Ultimately, these increased squamous epithelial cells were deposited on Buck’s fascia and formed an epidermal layer over it.
Ectopic tissues present in the human body such as endometriosis or ectopic pulmonary tissues are typically susceptible to infection [10]. While organs have specific immunity according to their characteristics [11], ectopic tissues do not have this specific immunity suited to the surrounding environment making them prone to infection [10]. Additionally, they can act as foreign bodies and cause inflammation. Ectopic tissues including ectopic epidermal layer on Buck’s fascia usually do not cause complications. However, the risk of complications increases dramatically for patients in conditions prone to inflammation [12]. In our patient, aggravation of diabetes was the trigger. The patient had no complications at the augmentation site for the past 17 years; however, as his diabetes worsened, extensive penile inflammation occurred. Immunocompromised conditions due to diabetes may have caused inflammation of the ectopic epidermal layer [12].
Complete surgical removal of the epidermal layer of a wound through en bloc excision is the most effective procedure for treating patients similar to our case. Debridement of the inflamed tissue alone is not sufficient. In this case, several debridements of the inflamed tissue were performed at the beginning. Various attempts including NPWT or nanocrystalline silver antimicrobial barrier dressings (Acticoat, Smith & Nephew) were additionally performed by us to clean the wound. However, the effect of these measures was limited. Because the wound was not healthy and clean enough to close, we had to perform en bloc excision of the wound to secure a clean wound and obtained satisfactory results. Total removal of the epidermal layer of the wound was also essential to prevent the recurrence of infection considering the patient’s weakened immunity. Any residual epidermal layer of the wound could not only promote infection, but also create new infection sources such as epidermal inclusion cysts or cholesteatomas [2,13].
Several cases of complications such as epidermal cyst formation or contour irregularity due to incomplete excision of the epidermal layer of dermofat graft were reported [13]. However, there have been no reports of cases in which the residual epidermal layer itself caused the inflammation. To the best of our knowledge, this is the first report of extended inflammation impending sepsis caused by the residual epidermal layers of the dermofat graft. Although the small number of reported cases makes it difficult to accurately determine the mechanism of inflammation, the inflammation had certainly initiated from the residual epidermal portion of the dermofat graft. It is important to perform a precise excision of the epidermal layer to prevent unexpected infection. Additionally, long-term follow-up for infection monitoring following dermofat graft is mandatory, especially in patients with underlying conditions such as diabetes. Even in patients who have been complication-free for extended periods, sudden inflammation may arise due to aggravation of the underlying condition [12]. If an epidermal layer of dermofat or wound base is suspected during the treatment of dermofat graft infection, confirmation of the presence of the epidermal layer through intraoperative biopsy and en bloc excision of the epidermal layer might be helpful.
Notes
No potential conflict of interest relevant to this article was reported.