Complete Bony Segment Flap Failure without Skin Paddle Compromise in Fibular Free Flap: A Case Report of a Rare Early Complication
Article information
Abstract
The free fibula flap is sometimes associated with partial flap loss. A 62-year-old man with squamous carcinoma of the lower alveolus underwent anterior arch resection and reconstruction with a fibula osteocutaneous flap containing three bony segments. There were two perforators in the skin flap; the first perforator was proximal to the bony segments and the other perforator was at the level of the middle segment. Atherosclerosis was observed in the anastomotic vessels. During surgery, thrombosis occurred in the arterial anastomosis, but was revised before the operation was over. The patient’s early postoperative course was uneventful. In the second week, purulent discharge was observed from the drains. Flap exploration showed devascularization of bony segments and periosteum, but the skin paddle was viable. The peroneal vessel had thrombosed distal to the takeoff of the proximal perforator and the viable skin paddle perfused by proximal perforators falsely indicated the well-being of underlying bones. The de-vascularized bones and sloughed periosteum were removed at the time of exploration, after which the skin paddle was reoriented for coverage of the defect. The patient completed chemoradiation without any bony reconstruction afterwards. This is the only reported case of early total bony flap portion loss with a viable skin paddle in free fibula flap transfer.
Introduction
While free fibula flaps are most commonly used for mandibular reconstruction [1], clinical monitoring of the skin flap portion for overall viability is not always reliable, especially for mandibular reconstruction involving multiple osteotomies. Partial or total loss of flaps also implies loss of cutaneous paddle and bone segments [2]. Total flap loss is usually characterized by discontinuity of flap perfusion secondary to events such as thrombosis, kinking and spasm [2]. While partial loss of skin flap is plainly visible, loss of vascularity of only bony segments is difficult to diagnose and usually presents later with non-union or sinus [3]. Though there are reports of early loss of cutaneous segments, we have not come across any case of early bone loss without loss of cutaneous segments. This paper reports a rare case of early partial free fibular flap loss involving only the bony part of the flap, sustaining viable skin. The patient provided written informed consent for the use and publication of his images.
Case
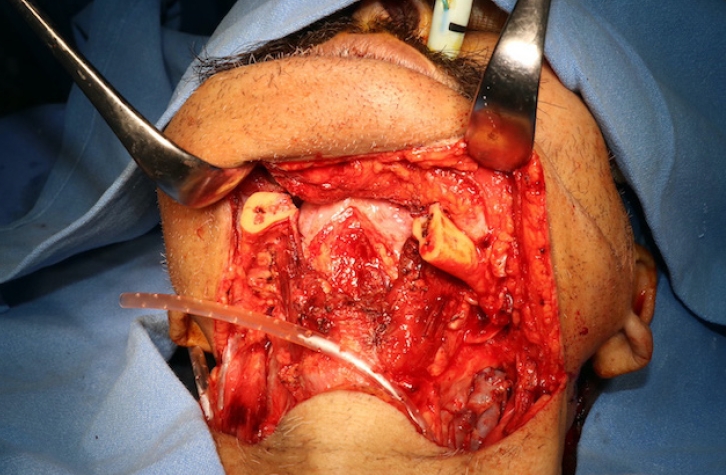
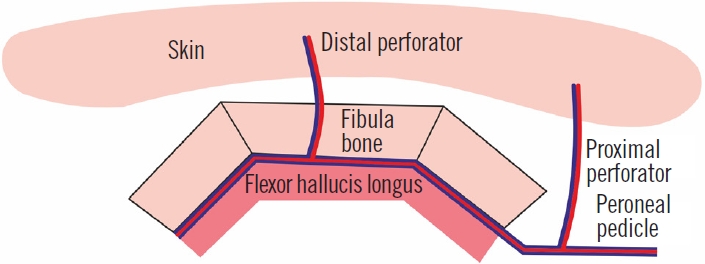
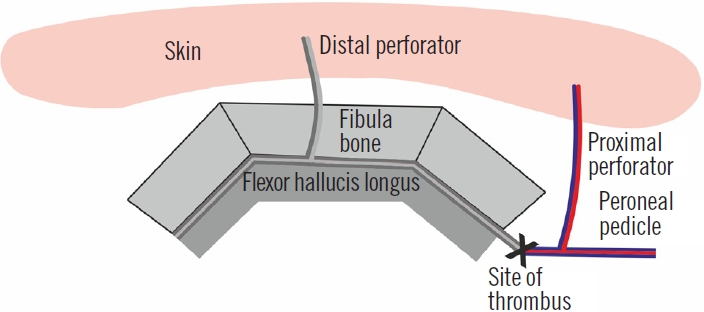
A 62-year-old diabetic patient presented with squamous cell carcinoma of the lower alveolus extending to the lower lip (Fig. 1). He underwent composite resection of the anterior arch of the mandible and full thickness of lower lip and chin skin (Fig. 2) along with bilateral neck dissection. Reconstruction was performed using a fibula osteocutaneous free flap with part of the flexor hallucis longus (FHL) muscle (Fig. 3). There were three osteotomized segments of fibula bone in the flap measuring 3.5, 3.2, and 3 cm, respectively. The skin paddle of the flap measured 14×6 cm. The overlying skin of the fibula flap had two perforators, one arising at the level of the middle segment and the other one directly from the peroneal artery proximal to the bony segments (Fig. 4). Anastomoses were performed to the facial artery and two branches of the internal jugular vein on the left side. Both the donor and recipient arteries had severe atherosclerosis. After initial anastomosis, the skin paddle did not show any bleeding from the skin margins, and the FHL muscle was also discolored. Thrombosis of the arterial anastomosis and absence of arterial pulsations distal to the anastomosis site were observed during the initial surgery. On excising the anastomosis site during immediate revision, a thrombus was identified. A 2 cm vein graft was interposed for tension-free arterial anastomosis, and the patient was put on therapeutic anticoagulation using enoxaparin 0.6 mL subcutaneously twice a day.
Postoperatively, the flap was healthy, and the patient was kept in the intensive care unit for 2 days for routine observation. He was managed in the inpatient ward afterwards. On day 10, the neck drains showed purulent output which did not improve even after escalating the antibiotics. The patient had been on cefoperazone sulbactam, which was escalated to piperacillin-tazobactam. The aerobic cultures from the drain were sent for microbiology. Culture report showed Escherichia coli, which was sensitive to the escalated drug. On day 13 the patient was taken up to the operation room for exploration as the purulence in the drains persisted although total leucocyte count and C-reactive protein levels were normal. There was pus and slough around the bony part of the flap. It was found that though the skin flap was healthy, all three bony segments were devascularized (Fig. 5). The periosteum over the fibular segments was also necrotic. The bones were removed and there was no bleeding from the edges. While pulsations of the proximal perforator perfusing the skin paddle were observed, no pulsations of the peroneal artery distal to takeoff of the proximal perforator were found (Fig. 6). The devascularized bones (Fig. 7), periosteum and FHL were discarded. The same skin flap was refashioned to cover the defect, after which the patient had an uneventful recovery. The patient refused any further bony reconstruction and completed his chemoradiation with the deformity (Fig. 8).
Discussion
Hidalgo in 1989 first used the free fibula flap for mandible reconstruction [4]. While being the most commonly used bony free flap for mandibular reconstruction, it is still associated with complications. The overall complication rates of the free fibular flap in literature range from 8% to 57% [5,6].
The complications can involve both donor and recipient areas [7]. Complications associated with the recipient area are graft survival problems, issues of incomplete reconstruction leading to inferior functional, aesthetic results and those related to recurrence of the primary pathology [8].
Flap loss can be partial or complete. Free fibula flap failure rates range from 4% to 12% for complete loss and 4% to 7.8% for partial flap loss [9,10]. The main characteristic of partial flap failure is continued blood supply by the vascular pedicle, as observed in this case. It is always tricky to manage partial fibular flap loss. Partial flap loss typically involves only skin flaps [2], and there are very few reported cases of bone-only loss maintaining intact skin paddles. These bone-only losses are found in the late postoperative period (usually after months or years) after completing radiotherapy and are usually due to osteoradionecrosis [10]. In their 190 cases of fibula flaps over 19 years, Knitschke et al. [2] had bone-only loss without skin paddle involvement at an average of 181 days after surgery, while there were no losses in the early postoperative stages. In addition, such bone loss involves only part of the bone segments. This can be managed by removing the affected part, risking some functional and aesthetic loss, which may or may not require further reconstruction. Bone scans can diagnose devascularization of bony segments both in the early and late stages. Schuepbach et al. [11] reported the advantages of early bone scans after mandibular reconstruction. Of the six cases of free scapula flaps included in their study, two cases did not display uptake of radioisotope in bone even though there were viable skin paddles 12 hours after the surgery. Both cases had arterial thrombus which were revised, and the flaps were salvaged only because the thromboses were picked up in time via bone scan.
While our patient suffered loss of all three bony segments, his skin was intact in the early postoperative period, which is a very rare finding. The first impression on observing the purulence in drains was that either there must be wound dehiscence in the posterior part (which cannot be easily inspected per orally), or that devascularization of the FHL muscle had occurred along the pedicle. As we did not suspect devascularization of the bony segments, imaging modalities such as bone scans were not performed. The possible explanation for this event could be an embolus from the site of anastomosis that had dislodged and blocked the vessel just distal to the origin of the proximal perforator. The ischemia most likely led to destruction of the periosteum over the bones and bone loss as the bony segments of fibula were perfused by periosteal blood supply. The skin paddle used for coverage of the defect and also for monitoring was perfused well due to the intact proximal perforator, but it did not reflect the condition of the underlying bones. Hence early partial bone-only free fibula flap loss can take place notwithstanding an intact skin paddle. The case demonstrates that skin paddles used for monitoring of fibula flap may be misleading, particularly in patients with atherosclerosis.
Notes
No potential conflict of interest relevant to this article was reported.