Treatment of Partial-Thickness Burn Wounds with Combined Advanced Therapies: Cultured Allogenic Keratinocyte and Epidermal Growth Factor
Article information
Abstract
Background
Cultured allogenic keratinocyte (CAK) and epidermal growth factor (EGF) are commonly used biological treatments for partial-thickness burn wounds. A comparative study was conducted on whether the combination therapy of CAK and EGF promotes partial-thickness burn wound healing.
Methods
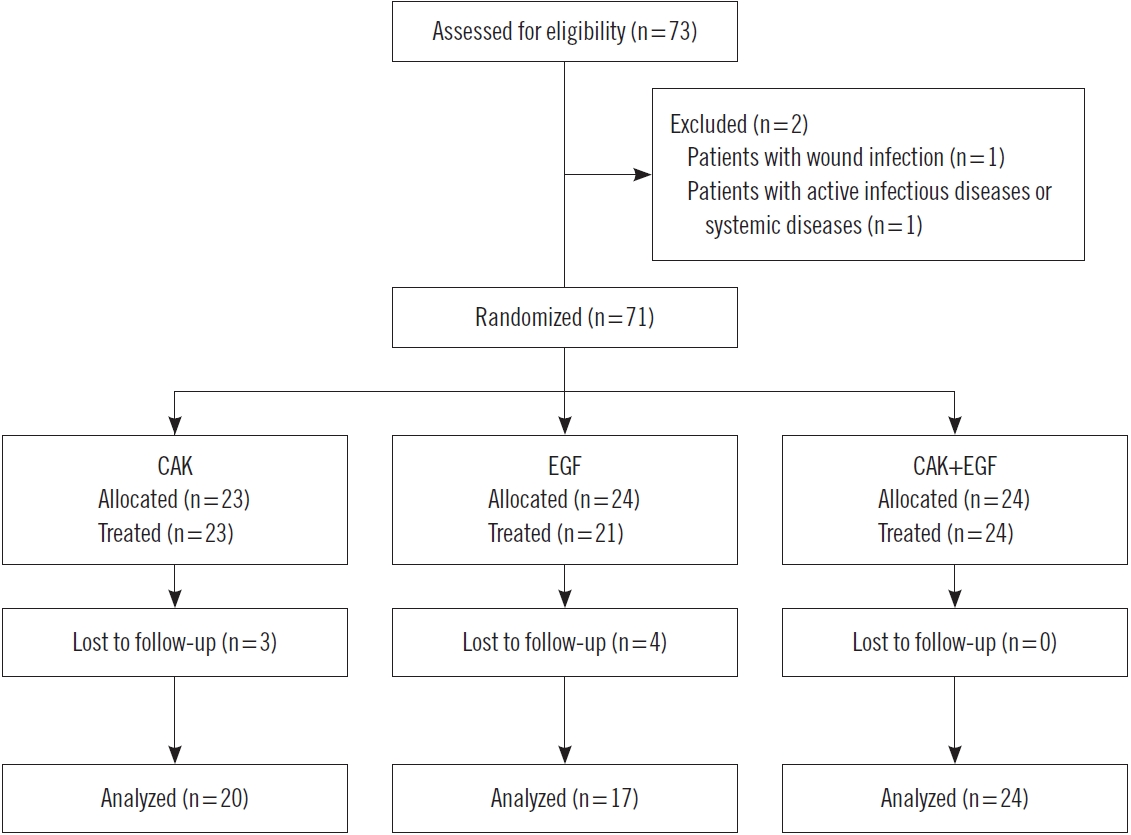
From January 2020 to March 2021, 73 patients who visited the hospital with partial-thickness burns were enrolled in the study. Patients were treated with CAK (Kaloderm) (n=20), EGF (Easyef) (n=17), and CAK+EGF (n=24). Wound healing rate, time to heal, factors affecting wound healing (age, sex, underlying disease, mode of injury, location of injury, initial wound size), and scarring were comparatively analyzed.
Results
The wound healing rate for 20 days was 85% (17/20) in the CAK group, 88% (15/17) in the EGF group, and 92% (22/24) in the CAK+EGF group. The average healing time was 11.0±6.0 days, with the CAK group taking 12.6±5.5 days, EGF group taking 11.5±6.0 days, and CAK+EGF group taking 9.0±6.3 days. The patients who received CAK+EGF treatment had higher hazard than the patients without CAK+EGF treatment (hazard ratio, 2.078; 95% confidence interval, 1.021–4.228). Smaller wound size <5 cm2 (hazard ratio, 2.869; 95% confidence interval, 1.426–5.773) was associated with complete wound healing. Though statistically insignificant (P=0.218), less scars occurred in the CAK+EGF group.
Conclusion
Combination therapy of CAK and EGF promotes wound healing in partial-thickness burn wounds.
Introduction
Partial-thickness burn wounds, which are burns from the epidermal layer to the dermal layer, are commonly seen in clinical practice [1]. Such wounds are not life-threatening and can be cured with standard wound care. However, if wound healing is impaired, it can lead to hypertrophic scarring which can significantly undermine the quality of life [2]. For treatment of partial-thickness burns, whether surgery should be performed at an early stage or delayed until dermal components are regenerated is often not easy to determine. In 1983, Engrav et al. [3] concluded that in dermal burns covering less than 20% of the total body surface area, early excision and grafting is the preferred treatment, as it results in less hypertrophic scarring. Recently, many studies have reported that conservative treatment using various advanced therapies is effective for partial-thickness burn wound healing [4-12].
Biological wound healing therapies are aimed at promoting wound healing [13]. Biological dressings prevent fluid loss, heat loss, and protein and electrolyte loss. They allow autolytic debridement and help develop granulation tissue. Such therapies include biological skin equivalents, growth factors, and tissue engineering.
Epidermal growth factor (EGF) promotes regeneration of damaged epithelium by acting on epithelial cells and fibroblasts [14-17]. EGF spray (Easyef) is a 0.005% solution consisting of 1 mL of recombinant human EGF (rhEGF) and 9 mL of solvent containing 20 mg of methyl parahydroxybenzoate [17]. rhEGF consists of 53 amino acids and is biologically equivalent to human EGF.
Cultured allogenic keratinocyte (CAK) derived from neonatal foreskin contains one billion epithelial cells on top of a single mesh-type Vaseline gauze. It secretes growth factors such as transforming growth factor beta, transforming growth factor alpha, and basic fibroblast growth factor, and promotes wound healing by synthesizing and secreting fibronectin, laminin, thrombospondin, and extracellular matrix proteins involved in epithelial adhesion and migration [4,7,11,18].
CAK and EGF are commonly used biological wound healing therapies in partial-thickness burn wounds [4,7,12]. While the therapeutic effect of each component is well known, the combined effect of these two has not yet been verified. This study was conducted on the premise that combination therapy with CAK and EGF can better promote wound healing than applying them separately.
Methods
This study was designed as a prospective, randomized clinical trial to evaluate the efficacy of combination therapy with CAK and EGF in partial-thickness burns. From January 2020 to March 2021, 73 patients with partial-thickness burn wounds were enrolled in this study. Patients with wound infections, active infectious diseases, or systemic diseases that may interfere with treatment were excluded. Informed consent was obtained from all participants. The study was approved by the Institutional Review Board of Kyung Hee University Hospital (IRB file No: 2022-07-021).
Patients were randomly classified into groups using CAK, EGF, and CAK and EGF (Figs. 1-3). CAK (Kaloderm, Tego Science) was applied until the wound was completely healed and replaced once every 5 to 7 days [4,11]. EGF spray (Easyef, Daewoong Pharmaceuticals) was applied once a day for 7 to 10 days [8]. All wounds received standard wound care such as proper cleansing and nonadherent dressings. On days when EGF-treated patients did not visit the hospital, they were instructed to carefully open the dressing and apply the EGF spray. In the CAK+EGF group, we did not remove the applied CAK and sprayed the EGF over the CAK.

A case treated with cultured allogenic keratinocyte. (A) A 76-year-old female patient sustained scalding burns on the right foot dorsum. (B) Seven days after treatment. (C) Complete healing after 9 days.

A case treated with epidermal growth factor. (A) A 53-year-old female patient sustained a friction burn on the right cheek. Deep dermis was partially exposed. (B) Complete healing after 7 days.

A case treated with combination therapy. (A) A 32-year-old female patient sustained scalding burns on the anterior chest. (B) Near complete healing after 9 days. (C) Complete healing after 8 weeks. Mild pigmented scar remained; no hypertrophic scar occurred.
The wounds were evaluated once every 2 days until recovery. After healing, the scars were evaluated once a month for 3 months. The wound size was measured by multiplying the width by the length. The primary endpoint was complete closure of the wound for 20 days, which means 100% re-epithelization with no wound discharge. The wound healing rate, defined as the percentage of the total number of patients who were completely healed by 20 days, and time taken to complete wound closure were measured. Changes in the size of the wound, overall healing rate, and time taken to complete wound closure were measured [16,17]. The scars were scored using the Stony Book Scar Evaluation Scale (5, excellent; 4, very good; 3, good; 2, fair; and 1, poor) at 3 months after healing.
Statistical analysis was performed using the SPSS software for Windows version 15.0 (SPSS Inc.). Continuous variables were compared using analysis of variance (ANOVA) or the Kruskal-Wallis test. Categorical variables were compared using the chi-square test or Fisher exact test. The time taken for wound healing was compared using Kaplan-Meier analysis. Multiple covariates were evaluated using the Cox regression analysis. Statistical significance was set at P<0.05.
Results
Study population
The patients’ demographic data and wound characteristics are summarized in Table 1. Of the total of 73 patients, the study was carried out on 61 patients (20 received CAK treatment, 17 received EGF treatment, and 24 received CAK+EGF treatment) (Fig. 4). The mean age was 35.3±25.0 years and the male to female ratio was 32:29. The wounds were located on the face (n=23), upper extremities (n=16), lower extremities (n=18), and trunk (n=4). With regard to the mode of injury, 26 were friction burns, 18 were scalding burns, eight were contact burns, six were oil burns, and three were flame burns. There was no statistically significant difference in wound characteristics between the three groups. All wounds had deep partial-thickness burns, and in many cases, superficial and deep partial-thickness burns were mixed.
Wound healing rate and time to heal
Over the span of 20 days, 54 of the 61 patients had complete healing (89%). The wound healing rates (the percentage of the total number of patients who were completely healed by 20 days) were 85% (17/20), 88% (15/17), and 92% (22/24) in the CAK, EGF, and CAK+EGF groups, respectively. The average healing time was 11.0±6.0 days, with the CAK group taking 12.6±5.5 days, EGF group taking 11.5±6.0 days and CAK+ EGF group taking 9.0±6.3 days. Comparing wound healing time with one-way ANOVA analysis, the CAK group showed no significant difference from EGF group (P=0.681), and a significant difference from the CAK+EGF group (P=0.048) (Table 2).
Kaplan-Meier plot of time to heal
When Kaplan-Meier analysis was performed, excellent wound healing was observed in the EGF and CAK+EGF groups at the 20-day evaluation (Fig. 5). The probability of wound healing was significantly better in the CAK+EGF group than in the CAK group (log-rank test, P=0.042), and there was no statistically significant difference between the CAK and EGF groups (log-rank test, P=0.305).
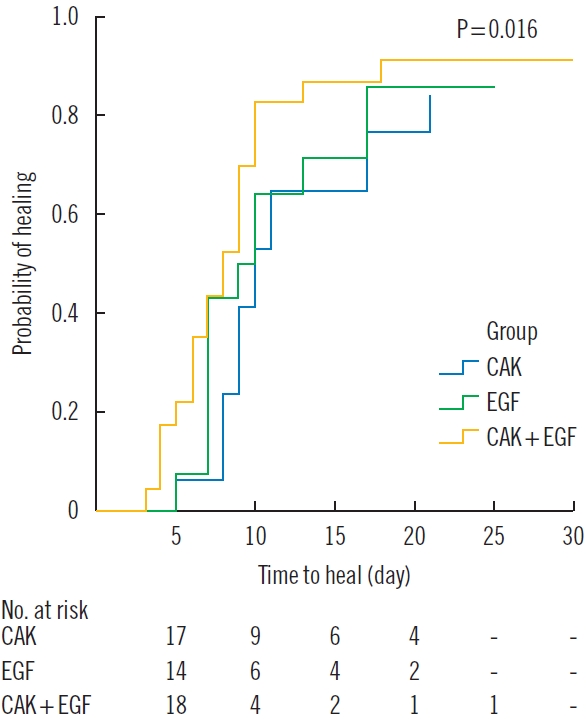
Healing ability differences between the three groups. Kaplan-Meier curve to compare healing ability differences according to CAK, EGF, and CAK+EGF groups. Differences between groups (CAK vs. EGF, EGF vs. CAK+EGF, CAK vs. CAK+EGF) were compared through log-rank tests corrected with Bonferroni post-hoc analysis.
Cox regression analysis
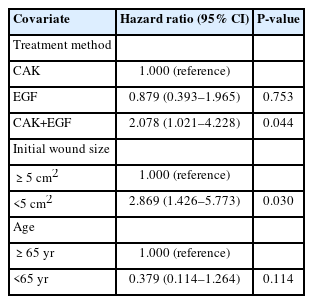
Cox professional hazard regression analysis was performed, and the following covariates were included in the first model: treatment method, age, sex, diabetes mellitus, hypertension, mode of injury, location of injury, and initial wound size. Two of these continuous covariates were changed to categorical variables for Cox regression: age: 1 (≥65 years), 2 (<65 years), and initial wound size: 1 (≥5 cm2), 2 (<5 cm2) (Table 3).
For the factors promoting wound healing, the patients who received CAK+EGF treatment were associated with better wound healing compared to those only with CAK treatment (adjusted hazard ratio, 2.078; 95% confidence interval, 1.021–4.228; P=0.044). Small wound size <5 cm2 (adjusted hazard ratio, 2.869; 95% confidence interval, 1.426–5.773; P=0.030) also was significantly associated with complete wound healing.
Scar analysis
Scarring occurred less in the CAK+EGF group than in other groups, although statistically insignificant (P=0.218). The scarring results at 3 months after healing were 4.0±0.7 points in CAK, 4.0±0.5 points in EGF, and 4.3±0.6 points in the CAK+ EGF group (Table 2).
Discussion
We evaluated the clinical outcomes of CAK, EGF, and CAK+ EGF treatments for partial-thickness burns. Wound healing took an average of 9 days in the CAK+EGF group, which was significantly shorter than that in the CAK (12.6 days) and EGF (11.5 days) groups.
Compared to previous research results, when CAK was applied to partial-thickness burn wounds, wound healing took an average of 12.9 days [4], which was similar to that in our study (12.6 days). When CAK was applied once to deep partial-thickness and partial full-thickness burn wounds, the average wound healing time was 13.4 days [7]. In another study, CAK was applied to facial burn wounds, and the average wound healing took 11 days [19]. It can be assumed that due to the characteristics of the facial area, which is rich in blood flow, wound healing took place more actively than in other areas, resulting in a slight reduction in time.
As for previous EGF studies, Wang et al. [9] demonstrated that partial-thickness burn wounds healed within 12.6 days using EGF ointment. In applying rhEGF ointments of 0.5 μg/g, 10 μg/g, and 50 μg/g once a day, 10 μg/g was the most effective. Liao et al. [8] applied 1 μg/g rhEGF ointment, and the average wound healing time was 13.7 days. Guo et al. [6] applied 1 μg/g rhEGF ointment to elderly patients aged 60 or older, and found that the average wound healing time was 20.5 days. The relatively longer healing times presented in their study were considered to be related to the fact that the study was targeted at elderly patients over the age of 60. In our study, EGF spray (Easyef) was used, which was a 0.005% solution consisting of 1 mL of rhEGF and 9 mL of solvent containing 20 mg of methyl parahydroxybenzoate. The spray was pumped twice for each treatment, and approximately 10 mg of rhEGF was pumped out in one pumping, which means that 20 mg was sprayed on the wound at a time. Compared to the ointment, the spray applied a much larger amount of EGF to the wound, resulting in faster treatment effects.
Research on the combination therapy of CAK and EGF has not yet been reported. The results of our study using combination therapy of CAK and EGF suggest that combination therapy can shorten the average wound healing time compared to when each is used separately. The complete healing rate within 20 days was 92% in the CAK+EGF group, which was higher than 85% in the CAK group and 88% in the EGF group (Fig. 5).
In general, CAK is applied once every 5 to 7 days, and in many cases, it is applied only once or twice. On the other hand, EGF may have worked better in that it could be applied daily. However, EGF is sprayed in liquid form; therefore, it does not fully remain on the wound surface when applied to specific curved areas. Meanwhile, CAK can adhere well to the wound surface and rarely falls off. It can also be inferred that spraying EGF on top of the CAK made it more likely to stay on the wound surface instead of running off, which could have made it more effective.
Wound healing is a complex multicellular process that ultimately aims to restore epithelium [20]. Multiple growth factors and cytokines play major roles in each process. Growth factors are a subclass of cytokines that stimulate cell differentiation [21]. Cytokines and growth factors perform the chemotactic activities of fibroblasts and inflammatory cells, promote angiogenesis, act as a mitogen to stimulate cellular proliferation, control the production of extracellular matrix, and modulate the synthesis of other cytokines and growth factors [22,23].
Because of the depth of partial-thickness burn wounds, hypodermal structures such as subcutaneous adipose tissue, connective tissue, and blood vessels usually remain under the wound bed. In this state, growth factors can work well for promoting wound healing.
In burn wounds, the longer the wound lasts, the more prominent the inflammatory response can be, which increases collagen deposition and aggravates the scar [24]. Eisinger et al. [25] also documented that covering the wound with epithelium reduces the scarring potential by down-regulating the inflammatory response, which is called the “epithelial-derived factor” and reduces the proliferation of fibroblasts. In the CAK+EGF group, scarring occurred less than in the CAK or EGF group, though the difference was statistically insignificant.
As for the shortcomings of this study, comparisons to determine the best ratio of CAK to EGF combination were not performed. As Zhang et al. [12] argued, it is important to determine the ideal dosage when performing growth factor therapy to maximize patient benefits, reduce costs, and achieve the best effect. Although this study used the most common dosage described in previous studies [4,6,11,15], further research may be necessary to determine which dose combination will have a greater effect. Second, while this study found that EGF+CAK treatment was more effective than standalone EGF or CAK treatments, it was not possible to compare the effectiveness of CAK+EGF treatment with that of the existing standard wound care. Third, the cost-effectiveness of CAK and EGF combination therapy was not evaluated. The financial strain on patients may increase because CAK and EGF sprays are relatively expensive therapeutic options. However, to minimize the financial burden on patients, EGF was billed in installments while CAK was covered by national health insurance. Clinical use might benefit from an analysis of cost-effectiveness and average cost increases based on the lesion. Fourth, the treatment was not assessed across different body parts. Since some body parts (such as the face) have more abundant blood flow than other parts, wound healing can be superior, which may lead to a difference in reactivity to growth factor therapy. Further studies on the effects of growth factor therapy for each site are required.
Notes
No potential conflict of interest relevant to this article was reported.