Verrucous Carcinoma of the Toenail: A Case Report and Review of Literature
Article information
Abstract
Verrucous carcinoma (VC) is a rare, highly keratinized, well-differentiated, low-grade squamous cell carcinoma. A 58-year-old male presented with a 5-year history of a recurrent growing hyperkeratotic mass with intermittent bloody discharge, ulceration and dystrophic nail change on the right fifth toe. Since multiple dermatologic treatments were yielding no response, punch biopsy was performed for a more accurate diagnosis and the result was consistent with verruca vulgaris. As the lesion was responding poorly despite further dermatologic treatments for verruca vulgaris, radical surgical resection was performed. Microscopic examination of the excised lesion revealed epidermis with hyperkeratosis, hypergranulosis, papillomatosis, and reticular dermis invasion, consistent with VC. Since the diagnosis changed to VC, and the resection margin was involved by the carcinoma, the patient underwent an amputation procedure at the proximal phalangeal base. This case report highlights the importance of diagnosing VC. In cases of lesions such as verruca vulgaris or onychomycosis that are not responsive to general treatment, physicians should consider VC as a differential diagnosis, to prevent delaying a proper diagnosis and progression of disease.
Introduction
Verrucous carcinoma (VC) was first described in 1948 as a slow-growing exophytic and papillary lesion [1]. VC is a rare, highly keratinized, well-differentiated, low-grade squamous cell carcinoma [2]. It usually originates from the plantar side of the foot, oropharynx, and genital area; distant metastasis is uncommon [3,4]. In most cases, preoperative diagnosis of VC is difficult because the outer layer of the lesion is usually covered by nonmalignant tissue [5], and the clinical presentation is often similar to other diseases, including keratoacanthoma, onychomycosis, paronychia, and verruca vulgaris. Here, we present a rare case of VC of the toenail that was initially misdiagnosed as verruca vulgaris. This case report highlights the importance of diagnosing VC via differential diagnosis of patients with keratinized toenail lesions to avoid unnecessary treatment and delayed diagnosis. The patient provided written in-formed consent for the publication and use of his images.
Case
A 58-year-old male presented with a 5-year history of a recurrent growing hyperkeratotic mass with intermittent bloody discharge, ulceration, and dystrophic nail change on the right fifth toe. The patient had a medical history of hypertension, atrial fibrillation, multifocal cerebral infarction, myocardial infarction with percutaneous coronary intervention, and epilepsy. Clinical examination revealed a non-tender, exophytic, hyperkeratotic lesion with thick plaque covering the whole single toenail with sanguineous oozing. This verrucous plaque involved the proximal nail fold, nail matrix, nail bed, and hyponychium. All his fingernails and other toenails appeared normal (Fig. 1).

Clinical photographs of the lesion. The patient presented with a recurrent, hyperkeratotic mass with intermittent bloody discharge, ulceration and dystrophic nail change on the right fifth toe. Punch biopsy was performed, and the lesion was diagnosed as verruca vulgaris. Clinical photos represent the lesion 2 years prior (A), 1 year prior (B), 6 months prior (C), and 1 month prior (D) to the operation, respectively.
Initially, the patient was clinically diagnosed with verruca vulgaris and received cryotherapy, which was not effective. Af-terwards, the patient was also prescribed topical antifungal agents and oral fluconazole for the possibility of onychomyco-sis; however, the lesion was non-responsive to these treatments. The patient was referred to our hospital to perform biopsy for a more accurate diagnosis. Punch biopsy was performed, and the histopathologic examination revealed a markedly papillomatous epidermis with parakeratosis, consistent with the findings of verruca vulgaris. The patient received further dermatologic treatment including cryotherapy, photo-dynamic therapy, topical diphencyprone application, local bleomycin injection, electrodessication, and CO2 laser for 2 years after his lesion was pathologically diagnosed as verruca vulgaris. However, as the lesion did not improve with these treatments, radical excision was planned after consulting with the patient, who had desired complete resection of the recurrent, poorly responsive lesion.
Under monitored anesthesia care, en bloc excision of the nail apparatus and distal phalangeal bony amputation was performed, and the fifth toe was reconstructed with a fillet flap (Fig. 2). A permanent biopsy was requested for the excised lesion. Intraoperative frozen biopsy was not performed since previous punch biopsy indicated a benign verruca vulgaris lesion, and therefore the possibility of malignancy was not considered. Microscopic examination revealed epidermis with hyperkeratosis, hypergranulosis, papillomatosis, and reticular dermis invasion, consistent with VC (Fig. 3). Since the diagnosis had changed to VC, and the resection margin was involved by the carcinoma, further wide excision was planned. Chest, abdominal, and pelvic computed tomography revealed no evi-dence of distant or lymphatic metastasis. Whole-body posi-tron emission tomography showed a possible malignant lesion at the plantar aspect of the right fifth toe proximal phalanx; otherwise, no definite abnormal findings were observed (Fig. 4). The patient underwent an amputation procedure on the right fifth toe at the level of the proximal phalangeal base (Fig. 5). Intraoperative frozen biopsy was performed for soft tissue, skin, and bone resection margin; none of these specimens was invaded by tumor. A final permanent biopsy showed VC-free surgical margins with no bone involvement, and the patient was discharged without any acute postoperative complications. The patient showed minimal functional impairment; no other complications or recurrence were observed at the 12- month follow-up.

Intraoperative photographs. (A) En bloc excision of the nail apparatus and distal phalangeal bony amputation was performed. (B) Excised specimen involving proximal nail fold, nail matrix, nail bed, and hyponychium. (C) The fifth toe was reconstructed with a fillet flap.
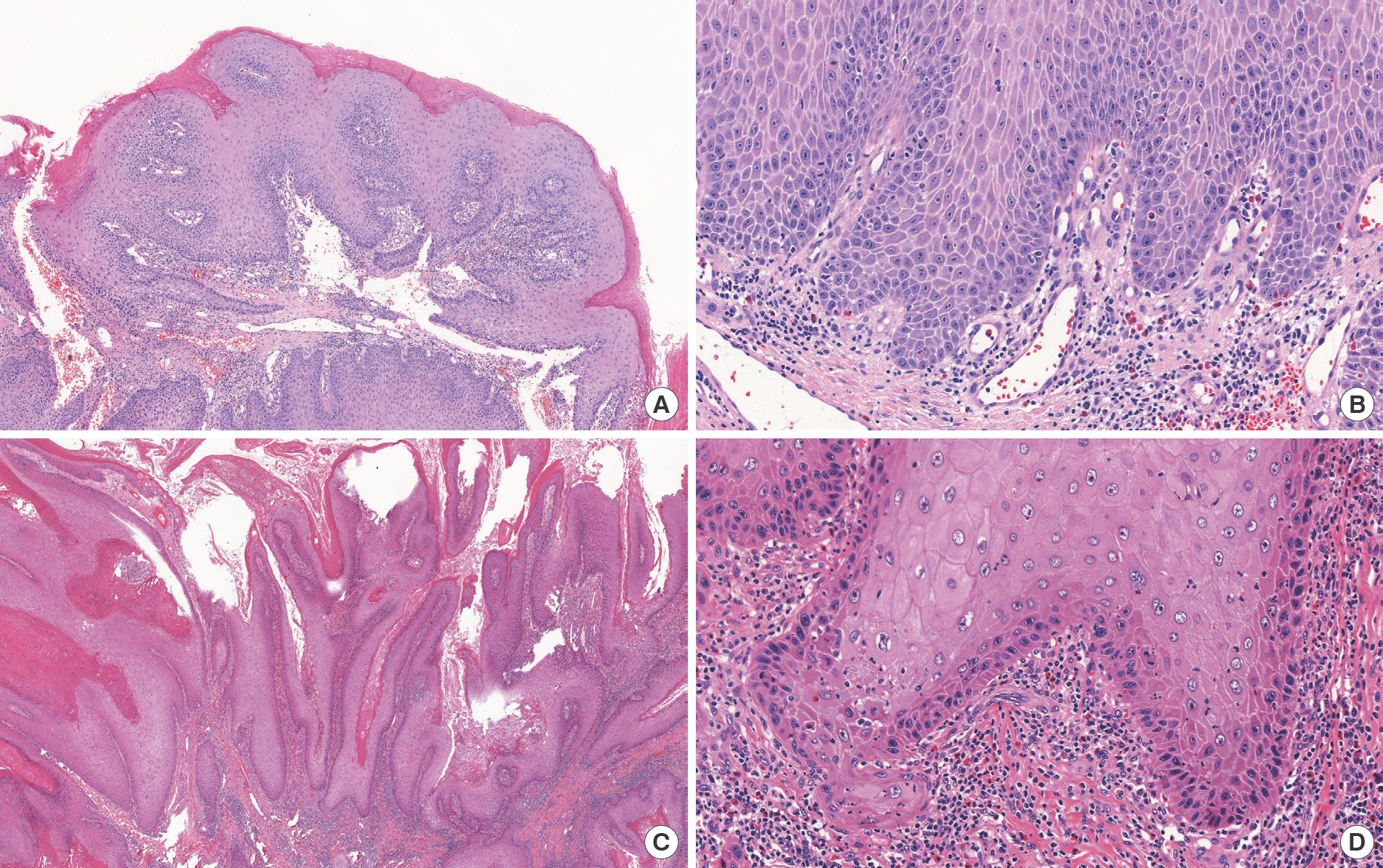
Histopathologic finding of specimens. (A, B) Punch biopsy specimen. Acanthotic squamous epithelium with mild papillomatosis are observed in the biopsy specimen. Cytologic atypia is minimal and some mitotic figures in the basal layer are also noted (H&E stain; A: ×40, B: ×200). (C, D) Surgical specimen. The specimen presented with marked verrucous acanthosis with broad bulbous growth pattern and reticular dermis invasion. Cytologic atypia is observed to a slightly higher degree with typical ground-glass cyto-plasm (H&E stain; C: ×20, D: ×200).

Positron emission tomography images. The image showed a possible malignant lesion at the plantar aspect of the right fifth toe proximal phalanx. (A, B) Axial image. (C) Coronal image. (D) Sagittal image.
Discussion
VC originates from various epithelial linings; the most com-mon location being the oral cavity, larynx, esophagus, and genitalia [3]. Some studies reported that the risk factors for oral VC were poor oral hygiene, smoking, and alcohol abuse [6]. VC is also known to occur in the hands or feet, especially in the sole area [7]. However, subungual VC is very rare, and a literature review retrieved 14 cases of VC involving the nail bed. Only eight of these cases originated from the subungual region rather than the fingers or toes.
McKee et al. [8] and Matoso et al. [9] reported finger VC originating from the subungual region. Dobson et al. [10] and Sheen et al. [11] reported VC originating from the thumb subungual area. Fewer cases originating from the toenails com-pared to cases from the fingernails have been reported. Van Geertruyden et al. [12] and Chaabani et al. [13] reported VC originating from a big toe nailbed, while Tosti et al. [14] described one patient with VC originating from the fifth toe and one with VC arising from the thumbnail bed. In most cases, a proper diagnosis was delayed due to a misdiagnosis or inappropriate biopsy specimen. A nail biopsy is essential to diag-nose VC and should include the reticular dermis for proper diagnosis [9]. In our case, histopathological examination of the initial punch biopsy specimen revealed acanthosis with mild papillomatosis of the squamous epithelium. Cytologic atypia was minimal, and dermal invasion was not observed. In the excised specimen 2 years after the first biopsy, much more prominent verrucous acanthosis was observed, and invasion of the reticular dermis was observed with a slightly higher degree of cytologic atypia, leading to a diagnosis of VC. The pa-thologist noted that the previous biopsy specimen did not cover the reticular dermis layer, so invasion of the reticular dermis could not have been observed.
The treatment modality for VC of the nail varies from local treatment such as cryotherapy, electrodessication, and curet-tage to wide surgical excision. Treatment options are deter-mined based on bone involvement and extend of lesion [9]. Local treatment of the tumor often fails, resulting in tumor recurrence. If there is bone involvement, amputation of the distal phalanx must be considered. For lesions without bone involvement, Mohs surgery is widely emerging and preferred because it preserves more tissue and distal function [12]. VC usually tends to show a less invasive and more indolent course than other skin cancers that originate from other parts of the body [13]. The clinical features of VC are non-specific and similar to those of benign lesions such as onychomycosis, paronychia, and verruca vulgaris. These indolent courses and non-specific presentations often lead to a delayed diagnosis. Delayed diagnosis can increase the risk of bony involvement and, therefore, can limit the treatment modality. In fact, due to delayed diagnosis and the physical contiguity between the nail bed and distal phalanx, bone involvement can be more easily seen in VC originating from the nail bed than from other sites [9,10]. Several cases without bone involvement showed suc-cessful digit salvage without amputation or cancer recurrence through wide excision of the lesion and reconstruction with a skin graft [8,9,14]. In our case, the cancer lesion was misdiagnosed as verruca vulgaris due to an inappropriate pathological specimen and non-specific findings. This delayed diagnosis led to the patient undergoing unnecessary surgery and a more destructive amputation operation. If the diagnosis had been made earlier, amputation at a more distal level or wide excision of nail or soft tissue with reconstruction for toe salvage could have been possible. However, the incidence rate does not justify biopsy or treatment intended for VC only based on first impressions. According to reports so far, VC is known as a cancer that demonstrates indolent growth. Since the general therapeutic effect of verruca vulgaris or onychomycosis appears after about 3 months, it is reasonable to consider biopsy for lesions that do not respond even after 3 months of general treatment.
In conclusion, we report a rare case of VC from the toenail. Though this case had not shown distal phalangeal involvement, an earlier misdiagnosis and delay in correct diagnosis had led to unnecessary destructive surgery. VC usually presents with non-specific features similar to other benign lesions. In cases of lesions such as verruca vulgaris or onychomycosis that are not responsive to general treatment, physicians should consider VC as a differential diagnosis.
Notes
No potential conflict of interest relevant to this article was reported.

