Reconstruction Using an Osteofasciocutaneous Fibula Free Flap for a Distal Tibial Defect in Refractory Chronic Osteomyelitis: A Case Report
Article information
Abstract
The fibular free flap (FFF) is an option used for tibial defect reconstruction in post-traumatic chronic osteomyelitis (PCOM). However, as the tibia is a weight-bearing bone, there exists a risk of compression fracture risk after FFF. This complicates reconstructing distal tibial defects adjacent to the articular cartilage. We report a successful case of reconstruction using FFF for a bone defect adjacent to the distal tibial articular surface in refractory PCOM. The patient was a 73-year-old woman with refractory PCOM in the right distal tibia secondary to a tibial fracture from a traffic accident that occurred 28 years ago. After bone debridement, the tibial bone defect was 8 cm in length, and its distal margin was located 0.5 cm above the articular surface of the tibiotalar joint. Tibial bone and soft tissue defects were reconstructed using a contralateral FFF consisting of an 8-cm fibula bone and a 14×5-cm-sized skin paddle. After 2 months, an Ilizarov apparatus was applied and maintained for 3 months. After 6 months, she started weight-bearing. The follow-up period was 15 months. Imaging studies revealed bone block union. The patient displayed no difficulty in ambulation and had no additional infections or flap necrosis.
Introduction
Management of post-traumatic chronic osteomyelitis (PCOM) includes infection control with surgical debridement, microbial-specific antibiotic administration, and soft tissue or bone defect coverage [1]. Reconstruction of bone defects consists of various techniques, including secondary intention wound healing, negative pressure wound therapy (NPWT), antibioticloaded polymethylmethacrylate beads, autologous bone grafts, and vascularized free bone flaps. Small defects can be replaced with autologous bone grafts from non-essential bones, such as the iliac crest. However, for larger defects, either distraction osteogenesis and the Ilizarov apparatus or vascularized bone flaps are better replacement methods [2]. The available donor bones for vascularized bone flaps include the ilium, fibula, scapula, and ribs [2]. The fibula has several characteristics of a good bone flap donor: sufficient length and high cortical density that allows it to withstand weight-bearing pressure [3,4].
The tibia is the most common site for PCOM [5]. For chronic osteomyelitis (COM), it is necessary to remove the infected bone tissue. For large tibial defects, contralateral fibular free flap (FFF) is a reliable treatment [6]. However, the tibia is a weight-bearing bone, with a larger distal weight distribution [7]. Therefore, one of the common complications of distal tibial reconstruction using FFF is a compression fracture of the re-cipient site after surgery [8]. For these reasons, reconstructing bone defects above the distal tibial articular surface is challenging and has been less reported. We therefore aimed to introduce a successful reconstruction case using FFF when refractory PCOM is present immediately above the distal articular surface. The patient provided written informed consent for the publication and use of her images.
Case
A 73-year-old woman underwent orthopedic surgery at another medical center for an open fracture of the right distal tibia and fibula following a traffic accident in 1992, after which osteomyelitis occurred. Despite six unsuccessful non-vascularized autologous iliac crest bone grafts (ICBG), PCOM continued to recur. In 2020, she was admitted to the department of orthopedic surgery of our institute because of pain and erythema at the previous surgical site. Laboratory test results showed normal white blood cell count and C-reactive protein levels but an increased erythrocyte sedimentation rate. Prior to admission in our hospital, she received 4 weeks of antibiotics in a local clinic. Subsequently, she underwent 2 weeks of antibiotic treatment at our hospital.
Plain X-ray images showed periosteal thickening, a central osteolytic lesion, and a cloaca, characteristics of COM, at the time of admission (Fig. 1A). Periosteal thickening, irregularity of the cortices, and a cloaca were also seen in the clinical image (Fig. 2A). Thorough wound debridement was performed to remove necrotized bone and soft tissue after removing the metal screws inserted at the previous medical center (Fig. 1B).
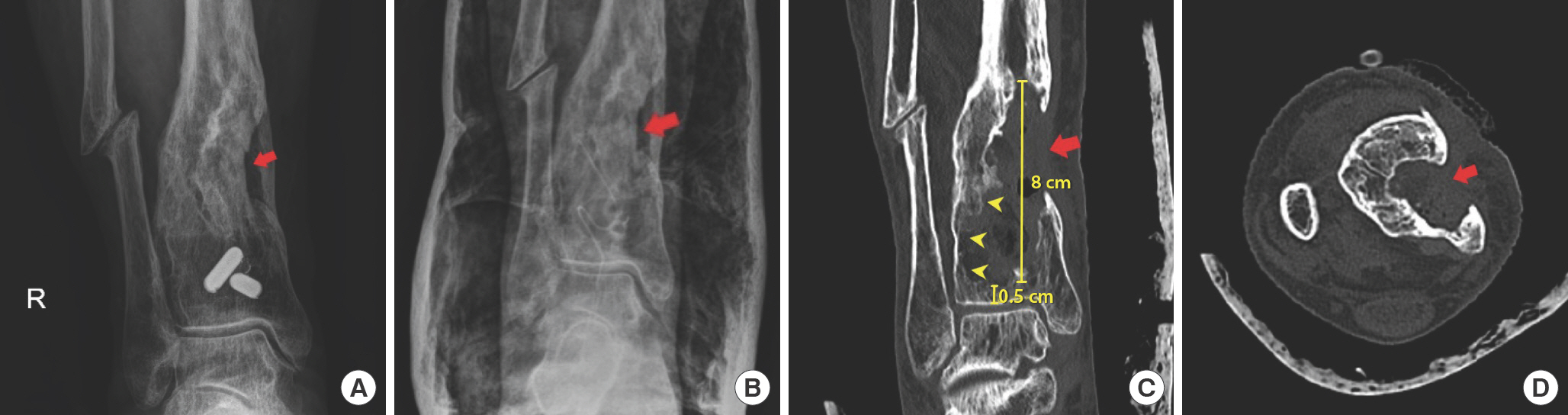
Preoperative clinical photos. A 73-year-old woman with 28-year post-traumatic chronic osteomyelitis of the distal tibia. (A) Anteroposterior (AP) view radiograph when she was admitted to the department of orthopedic surgery showing marked periosteal thickening, a central osteolytic lesion, irregularity of the cortices, and a cloaca (red arrow) of the right distal tibia. Fixation screws retained in the tibia are also visible, whereas the fibula displays non-union. (B) AP view radiograph, (C) coronal, and (D) axial computed tomography images after bone debridement and removal of the metal screws inserted from the previous surgery conducted at another medical center. A large bone defect in the medial portion of the distal third of the tibia with cloaca (red arrow) and sequestrum (yellow arrowheads) is observed. The bone defect is 8 cm in length, and its distal margin is located 0.5 cm above the distal tibial articular cartilage.
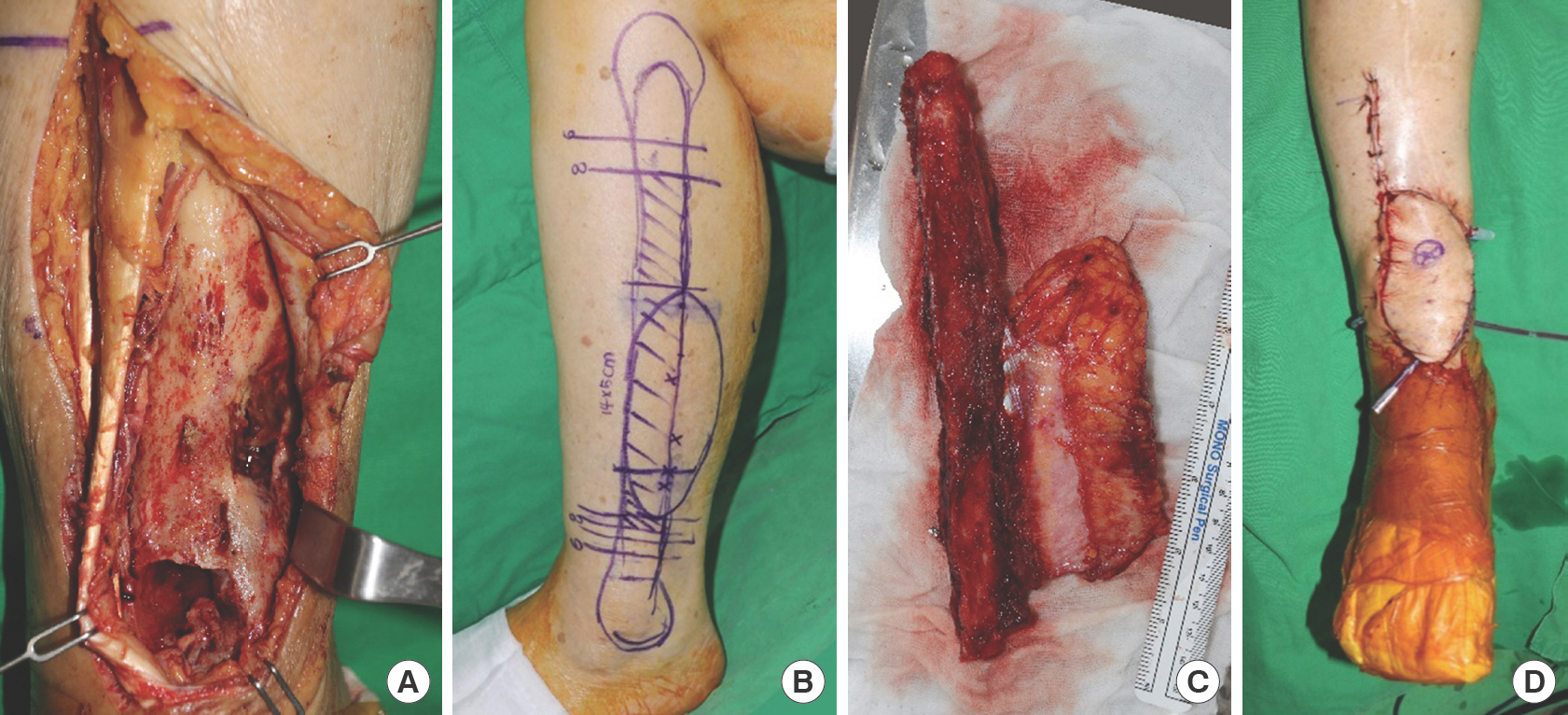
Intraoperative clinical images. (A) Necrotic bone of post-traumatic chronic osteomyelitis. (B) Fibula free flap design on the ipsilateral fibula. (C) Harvested flap with two perforators. The harvested flap consists of a 20-cm fibula bone and a 14×5-cm-sized skin paddle. The flap, including the distal 8-cm fibula, was used according to the defective length. (D) Postoperative image after insetting the flap.
Computed tomography images showed an 8-cm long bone defect in the distal tibia after bone debridement (Fig. 1 C and D). Moreover, the distal margin of the tibial bone defect was located 0.5 cm above the distal tibial articular cartilage; hence, she was restricted from weight-bearing and was only allowed wheelchair ambulation for stabilization. The patient was diagnosed with Cierny-Mader type III osteomyelitis of the right distal tibia [9].
She was then referred to the department of plastic and reconstructive surgery for bone defect reconstruction. As she had received 6 weeks of antibiotic therapy and bone debridement followed by NPWT, with no organisms in the wound culture, we considered that the infection was controlled. Computed tomography angiography revealed normal bilateral lower extremity vascularity. Therefore, we decided to reconstruct the bone and soft tissue defects with a contralateral vascularized osteofasciocutaneous FFF. The originally scheduled reconstruction surgery date was delayed owing to a medical personnel strike, which led to NPWT being prolonged for 7 weeks.
Our schematic surgical plan is shown in Fig. 3. We planned a two-team approach to reduce the operation time, performing the secondary bone debridement and flap harvesting at the same time. If diffuse osteomyelitis necessitated a wide range of bone debridement, we would split the bone flap in half perpendicular to its length and fold the two halves side by side to insert the bone flap in a “double-barrel” form (Fig. 3, part a). If only topical bone debridement was required for localized osteomyelitis, we would insert the bone flap as a “single-barrel” (Fig. 3, part b). The length of the bone to be harvested for the flap was twice that of the actual bone defect to allow for the double-barrel configuration.
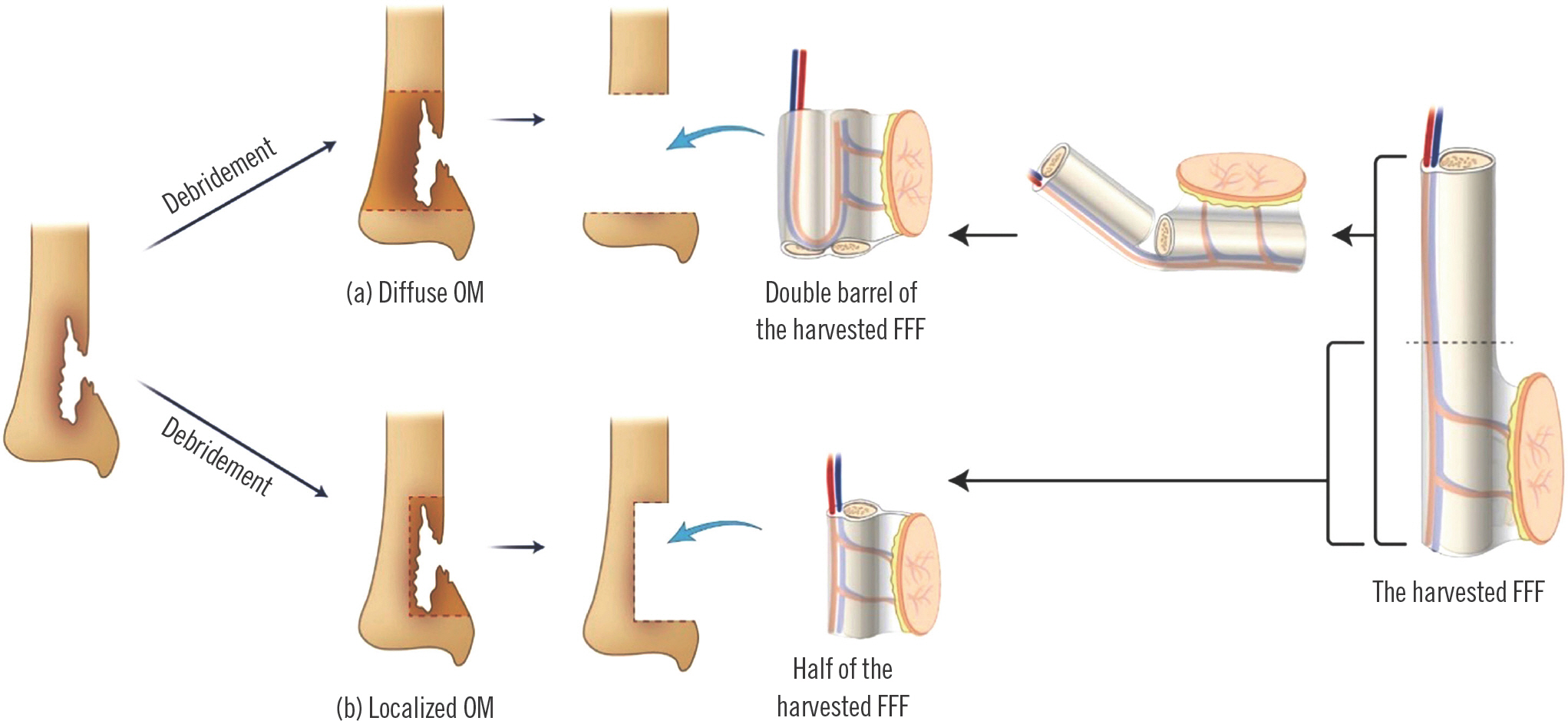
Surgical plan diagram. A fibular flap corresponding to at least twice the length of the tibial defect was harvested. (a) If osteomyelitis (OM) is diffuse, the bony portion of the harvested flap is split in half, perpendicular to its length, and the resulting struts form a “double-barrel” to cover the defect. (b) If OM is localized, the bony portion of the harvested flap is cut in 8 cm, perpendicular to its length, to cover the defect. FFF, fibular free flap.
We harvested a flap consisting of a 20-cm fibula bone strut and a 14×5-cm-sized skin paddle, connected to two perforators (measuring 13 cm and 10 cm from the pedicle, respectively) (Fig. 2B and C). Simultaneously, using a two-team approach, we debrided a small amount of nonviable remnant and infected tissue, including skin, soft tissue, and bone. De-bridement was performed until viable tibia was identified by inspecting for punctuation bleeding (i.e., “paprika sign”). After bone debridement, the osteomyelitis was not circumferential on the cross-section (Fig. 2A). As a result, the required bone flap length was 8 cm, similar to the defective length. The distal 8-cm portion of the fibula harvested with the flap was used, with the remaining bony section discarded. The peroneal artery of the flap was anastomosed end-to-side with the right anterior tibial artery, and the two accompanying veins of the flap were anastomosed end-to-end with the two vena comitantes of the right anterior tibial artery. The bone was stabilized via internal fixation using plates and screws. Fig. 2D shows the immediately postoperative image after insetting the flap. A split skin graft was performed to cover the lateral margin of the flap and the donor area remaining after primary repair. A fluffy gauze dressing was placed at the flap site, and a short leg splint was applied at the flap and donor sites.
As the intraoperative microbiological cultures were negative, culture-directed antibiotic treatment was not required. First-generation cephalosporin antibiotics were administered intravenously for 2 weeks and orally for 2 more weeks. On postoperative day 13, the flap was stabilized, and the patient was discharged from the hospital, wherein she maintained non-weight-bearing ambulation at the surgical site.
After 2 months, the flap remained stable (Fig. 4), and closed reduction and internal fixation with an Ilizarov apparatus (and Kirschner wire fixation above and below the osteomyelitis site) were performed to stabilize the distal tibia. After 3 months, a pin site infection occurred, which was improved with antibiotic treatment; culture-specific antibiotics (i.e., piperacillin and tazobactam) were administered intravenously for 8 days, and first-generation cephalosporin antibiotics were administered intravenously and orally for 3 weeks. After 5 months, the Ilizarov apparatus was removed. After 6 months, she started weight-bearing. Eight months later, imaging studies showed bone block union (Fig. 5A).
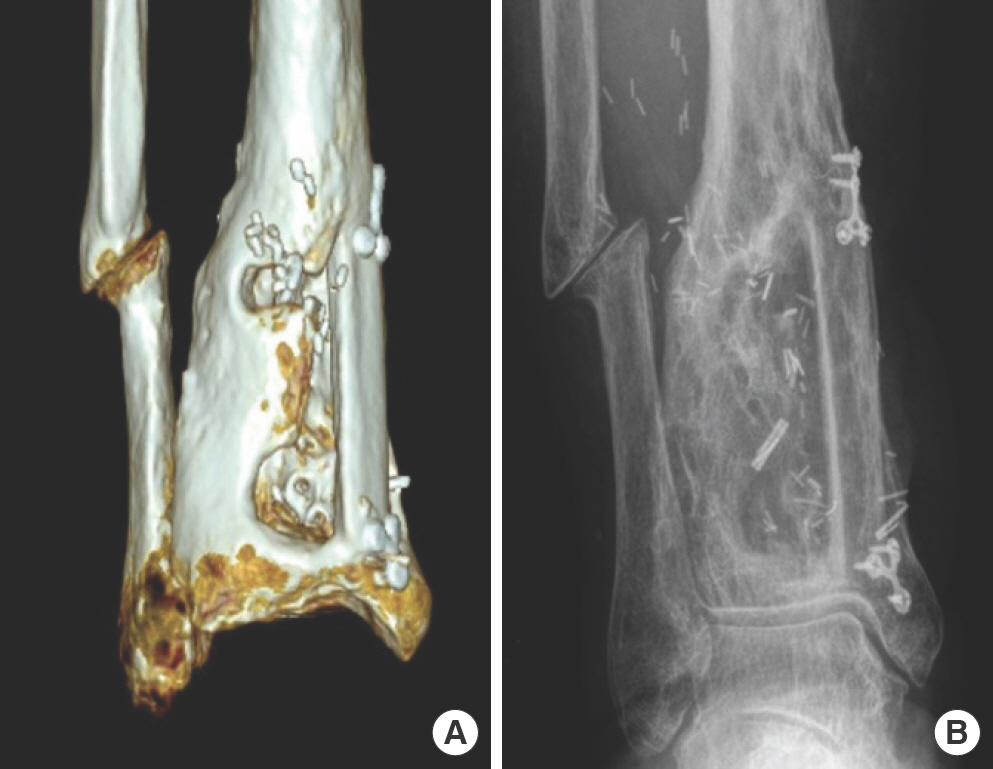
Postoperative imaging examinations. (A) After 8 months, bone union is observed in the three-dimensional computed tomography image (anterior side). (B) After 15 months, good alignment in the plain radiograph.
The follow-up period was 15 months (Fig. 5B). The patient could perform ambulation without orthosis 14 months after the surgery. No signs of recurrent infection or flap necrosis were observed. Applying the Stanmore System to assess final post-reconstructive ankle function, the patient's total score was 79, indicating a “good” result [10].
Discussion
Except for hematogenous osteomyelitis, which occurs mainly in children, most cases of osteomyelitis are post-traumatic and often occur due to open fractures and metal fixation surgery. In the acute form, approximately 10%–30% become chronic. PCOM is a disease that causes significant morbidity and can threaten limb viability [11].
Symptoms of PCOM may include localized pain, redness, swelling, drainage, and wound infection at the fracture site. Persistent non-union and delayed wound healing are typical symptoms of osteomyelitis due to open fractures. Symptoms such as fever and chills do not usually occur because such systemic symptoms are only present when bacteria are present in the blood. COM is characterized by frequent local bone loss, periosteal formation, and bone sclerosis. In addition, persistent drainage or sinus tract formation often occurs around the infected tissues. In the present case, the patient's symptoms included pain and redness. Moreover, the erythrocyte sedimentation rate was elevated, but the white blood cell count was normal in the laboratory results, as in the case of most COM.
To date, there are no evidence-based guidelines for the treatment of COM [12]; options include a combination of antibiotics, surgical debridement, and dead space management. However, even with good treatment outcomes, osteomyelitis can occur several years after the initial onset.
An important aspect of COM treatment is dead space management; if this is inappropriate, it can cause early recurrence of osteomyelitis. Bone defects less than 6 cm can be replaced with autologous bone grafts. For larger defects, using an Ilizarov apparatus or vascularized bone flap is preferred [13]. In a 2013 study by Abdel-Razek and Semaya [14], vascularized FFF had faster bone union and fewer wound complications than Ilizarov bone transport in patients with post-traumatic tibial bone defects. Furthermore, a well-vascularized bone flap has stronger resistance to infection than a non-vascularized one.
In our case, we considered additional ICBG as an ineffective treatment option for the patient because refractory osteomyelitis had already been treated with ICBG six times but continued to recur. In addition, owing to its large size, an 8-cm bone defect requires replacement with vascularized bone flap. However, since all the previous bone graft donors were iliac bones, a superficial circumflex iliac artery perforator free flap was no longer feasible; instead, we decided to use the fibula as the bone flap donor. As the fibula is a non-significant weight-bearing bone, it is used for reconstruction of bony defects in other parts of the body, including the tibia.
The Stanmore System used in this case for postoperative functional assessment of the lower limb was originally devised as a method for evaluating the functional results of postoperative posterior tibial tendon transfer or functional muscle transfer [10]. Since there is no accurate standard evaluation tool for evaluating function after vascularized bone replacement for distal tibial defects, we used the Stanmore System to evaluate ankle function. The categories of the Stanmore System are pain, need for orthosis, ability to wear normal shoes, functional outcome, muscle power, degree of active range of motion, and foot posture [10]. The patient's scores were 10 out of 15, 15 out of 15, 5 out of 5, 6 out of 10, 20 out of 25, 20 out of 25, and 3 out of 5, respectively, with a total score of 79.
This study has several limitations. First, there is the possibility of recurrence after the follow-up period. However, in the 15 months of our follow-up period, there was no recurrence of infection, the patient was able to ambulate, and the result of the functional evaluation according to the Stanmore System was “good.” Therefore, we considered this to be a successful case. Second, the period until ambulation was achieved was prolonged. The time to reach ambulation, in this case, was 14 months. As our patient had a high risk of articular fracture, we considered that external fixation with an Ilizarov apparatus was required. Flap surgery and external fixation were not simultaneously performed because if flap revision was necessary, it would be complex and difficult to proceed between the frame structure of the Ilizarov apparatus. We believe that it was better to apply the Ilizarov apparatus after the flap was first stabilized. Third, more than half of the harvested FFF was discarded. Fourth, due to the patient's age, there were concerns regarding her cardiopulmonary function during extended general anesthesia; therefore, methods to save surgical time were required. We determined a two-team approach to save surgical time.
To date, this is the first report of the reconstruction of a bone defect just above the articular surface of the distal tibia. Moreover, in this case, the patient had fibula non-union. Although the fibula is not the main weight-bearing bone, it supports the tibia and helps stabilize the ankle. For this reason, the weight load of the tibia was further increased in this case, thus increasing the risk of postoperative articular fracture.
No acute complications occurred immediately after surgery. After 15 months, bone union at the surgical site was radio-graphically evident (Fig. 5B), and there were no signs of recurrent infection or necrosis of the flap. In addition, the patient had ambulation without aid, and the functional evaluation was good. In conclusion, FFF could be considered as an option for the reconstruction of refractory PCOM, even in the case of a tibial defect adjacent to the distal tibial articular cartilage.
Conflict of interest
No potential conflict of interest relevant to this article was reported.

