Spontaneous Zone III Flexor Tendon Rupture of the Little Finger: A Case Report
Article information
Abstract
Closed flexor tendon ruptures are uncommon, and most are avulsion ruptures from the tendon insertion. Such intratendinous ruptures are generally associated with an underlying pathological process such as inflammatory disease; purely spontaneous ruptures are very rare. A 66-year-old male patient presented with sudden loss of flexion in the left little finger distal interphalangeal joint (DIPJ) while rotating a steering wheel. Preoperative ultrasonography and magnetic resonance imaging (MRI) suggested a closed flexor digitorum profundus (FDP) injury in the substance of the tendon. Surgical exploration revealed a zone III rupture in the FDP tendon. After tenorrhaphy, early postoperative exercise using a dynamic splint was initiated. At 8 months’ follow-up, he had regained flexion of the DIPJ and was free of pain. We recommend that patients with suspected closed flexor tendon injuries promptly undergo preoperative imaging studies such as ultrasonography or MRI to determine the rupture site, facilitating preoperative planning and reducing surgical morbidity.
Introduction
Closed flexor tendon rupture is an uncommon condition that may be caused by iatrogenic factors, inflammatory processes, direct trauma, or attrition, the last of which may result from various abrasive fulcrums or protrusions such as scaphotrapeziotrapezoid osteoarthritis, wrist fractures or dislocations, and hook of hamate fractures [1]. However, when tendon rupture occurs secondary to inflammatory processes, surrounding synovial infiltration is often found, potentially implying that the rupture was caused by inadequate management of the underlying disease. Isolated terminal avulsions of the flexor digitorum profundus (FDP), more common than ruptures in the tendon body, are often referred to as “jersey finger,” a term that reflects the tendency for this injury to occur when an athlete is holding onto the jersey of an opponent as the opponent pulls away, forcibly extending the flexed finger [1]. An elevated risk of tendinopathy and tendon rupture is associated with some classes of drugs, including most notably fluoroquinolones; the pathological processes underlying this highly infrequent phenomenon remain poorly understood, although microscopic alterations have been reported [1,2]. However, as closed intratendinous flexor tendon ruptures can occur even without any underlying pathologic problems, clinicians should be aware of these rare injuries to ensure that suitable investigations are carried out and also that unnecessary incisions and scarring are avoided, thereby improving patient care. We hereby introduce an extremely rare case of spontaneous intratendinous flexor rupture. The patient was informed that this case study would be submitted for publication and provided informed consent.
Case
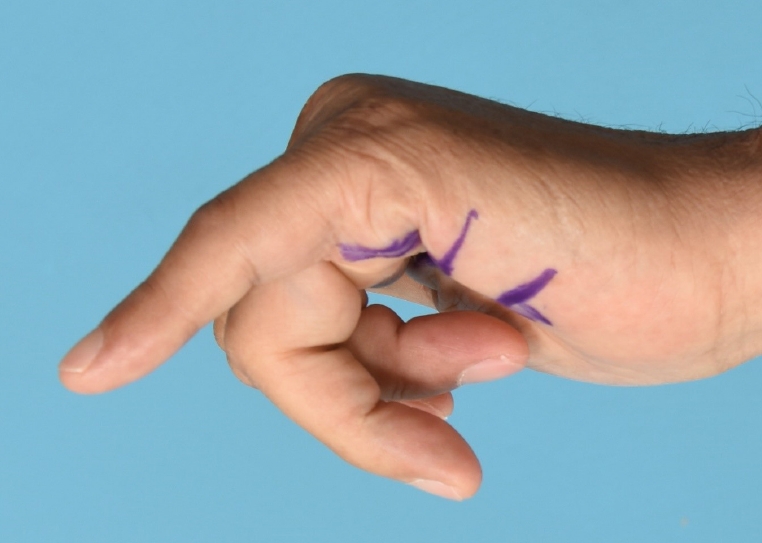
A 66-year-old man with right-hand dominance was referred to our clinic for loss of flexion in the left little finger. The patient explained that cramping and pain in the palmar area occurred a week earlier while he was using both hands to rotate the steering wheel of his car. The pain resolved shortly, but he immediately experienced an inability to flex the distal interphalangeal joint of his left little finger (Fig. 1). The patient maintained full range of motion of the proximal interphalangeal and metacarpophalangeal joints. He reported no previous experiences of discomfort or difficulty when flexing this finger, as well as no prior history of trauma or previous injections in the hand or wrist. The patient was a non-smoker and was otherwise healthy, with unremarkable findings on plain radiographs and blood tests including rheumatologic labs. Clinical examination 1 week after trauma showed an absence of bruising. Based on suspicion of a closed FDP tendon avulsion injury, magnetic resonance imaging (MRI) and ultrasonography were performed (Figs. 2, 3). The level of tendon rupture was identified in the palm, verifying the need for surgical exploration and repair. A zigzag incision was made over the patient’s left palm. Intraoperatively, rupture of the FDP tendon was observed in zone III at the origin of the lumbrical muscles, without any signs of the tenodesis effect (Fig. 4). The ruptured tendon stumps were sheared off in a slightly oblique configuration, with no visibly apparent diminution of the tendon body diameter. The proximal stump had retracted roughly 1cm from the distal stump, as predicted through preoperative imaging studies. No signs of synovitis or attrition were noted, and no sharp edges were observed in zone III. Four-strand double modified Kessler core repair with 4/0 Ethibond sutures and simple running epitendinous repair using 6/0 Prolene sutures were performed to repair the rupture. An early active motion flexor tendon protocol was implemented postoperatively. At an 8-month follow-up, the repaired tendon was found to be intact, with improved active range of motion at the distal interphalangeal joint (metacarpophalangeal joint: 0°–70°, proximal interphalangeal joint: 0°–80°, distal interphalangeal joint: 0°–50°) and no pain during gripping, but limited grip strength (Fig. 5).
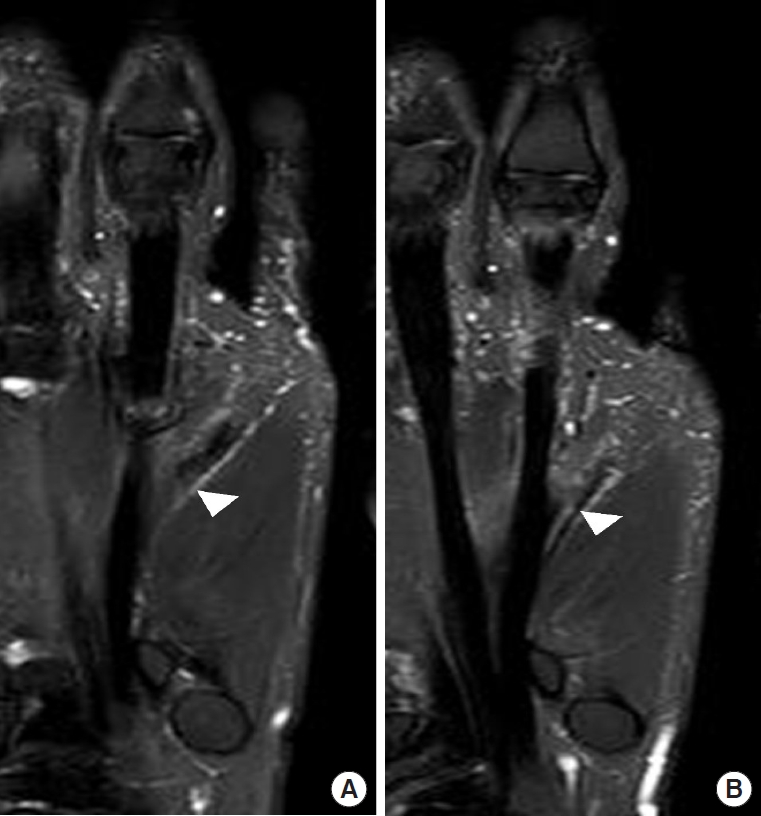
Preoperative T2-weighted magnetic resonance imaging. The distal (A, white arrowhead) and proximal (B, white arrowhead) ends of the ruptured flexor tendon are displayed.

Ultrasonography taken 12 days after injury. The distance between proximal and distal ends of the ruptured tendon was measured to be approximately 1 cm.

Intraoperative photograph, surgical exploration of hand. Rupture of flexor digitorum profundus tendon at origin of the lumbrical (black arrowhead).
Discussion
The term “spontaneous tendon rupture” was first used by Boyes et al. in 1960 to describe closed intratendinous rupture with no obvious intrinsic pathological mechanism, such as a tumor, infection, bony abnormality, or rheumatoid arthritis [3]. Regardless of the location of tendon disruption, trauma to the hand or wrist is the most frequent cause of closed flexor tendon ruptures. Avulsion of the FDP tendon at the bony insertion of the distal phalanx, the most common form, usually occurs when active flexion is performed against a source of resistance. This pattern can be interpreted in light of McMaster’s research, according to which the tendon is the strongest component of the musculotendinous unit [4]. The rarity of the case presented in this study is further underscored by Boyes et al. [3] who described 80 closed tendon injuries that occurred over the course of 13 years and found that 68% of those injuries occurred at the musculotendinous junction, while only 32% occurred within the substance of the tendon; furthermore, only 3.7% accounted as spontaneous ruptures [5,6].
The mechanism of the rare circumstances of spontaneous closed intratendinous flexor tendon rupture have not been completely elucidated. Similar to the case described herein, four of the five cases of spontaneous rupture described by Bois et al. in 2007 [6] involved ruptures in zone III of the little finger. Naam [7] also reported that 92% of the 13 spontaneous ruptures of their case series occurred in the palm, at the lumbrical level. These injuries present with diverse clinical manifestations; most affected patients report a popping sensation, although others—as in this case—may experience pain or cramping [1,6]. According to Imbriglia and Goldstein [8], the little finger FDP absorbs proportionately more stress load with less assistance from the flexor digitorum superficialis tendon (which may be absent) compared to the other digits; this may help explain the predilection for spontaneous FDP ruptures in the little finger. In the majority of reported cases, longitudinal force or flexion against resistance was involved at the time of injury [6,8], as in our case which occurred while twisting an automobile steering wheel. Although the details remain unclear, the underlying pathophysiology is likely to be multifactorial and to involve microscopic alterations. In a 1991 study, Kannus and Jozsa [2] found characteristic degenerative histopathological changes in 97% of tendon specimens obtained from various sites in 891 patients who had sustained spontaneous tendon ruptures. The most common pattern was hypoxic degenerative tendinopathy (44%), while other findings included calcifying tendinopathy, tendolipomatosis, and mucoid degeneration.
Arthritis, exostosis of bony surfaces, gout, synovitis, and chronic use of steroids can all act as intrinsic factors predisposing tendons to closed rupture. In our case, however, preoperative lab results and radiographs showed negative findings for chronic disorders, and intraoperative tissue samples were not sent for a histological analysis. In subsequent cases, histological samples should be obtained.
MRI and ultrasonography can both support the diagnosis of closed flexor tendon rupture. These imaging modalities also provide additional information on the location of the injury, tendon integrity, and the distance between the tendon ends. The interval between the occurrence of the injury and ultrasonography may have an impact on diagnostic accuracy; performing ultrasonography on the same day as the injury yields the most accurate results, underscoring the importance of a prompt evaluation [9]. In this case, preoperative ultrasonography and MRI was used to mark the level of the rupture, enabling easy intraoperative location of the tendon ends (Fig. 6). Regardless of the cause of rupture, the optimal treatment is early surgical repair and postoperative exercise. Recovery of full range of motion and grip strength was presumably hindered by poor postoperative compliance by the patient, rather than by the 2-week delay in surgical exploration. In chronically delayed cases, tendon transfers or grafts may be required for successful functional reconstruction [10].
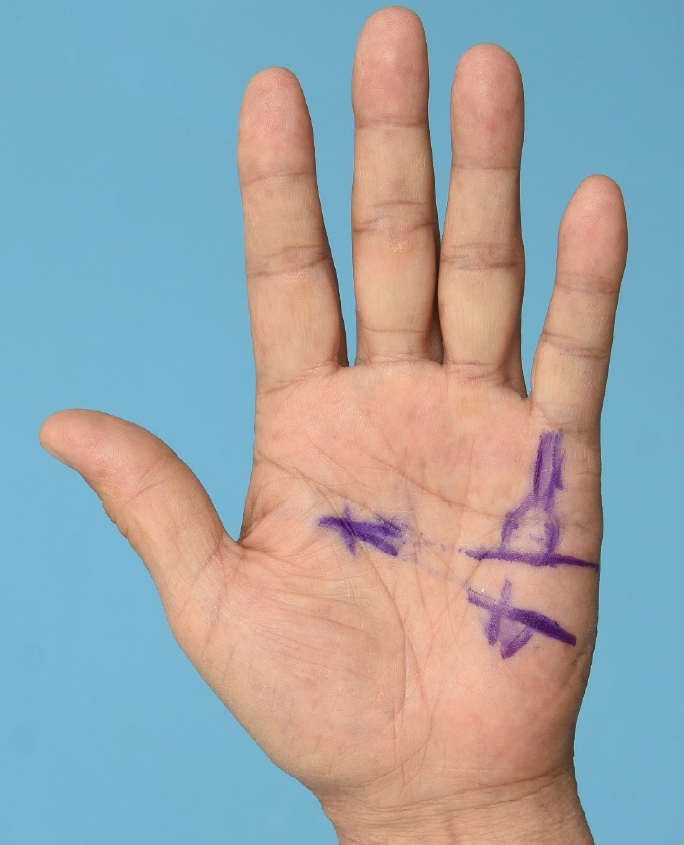
Presumed level of rupture. Preoperative ultrasonography was used to mark the location of the ruptured tendon ends.
Since spontaneous FDP tendon rupture within the tendon substance is quite rare, it may be challenging to diagnose. Unrecognized injuries may result in inadequate splinting and immobilization of the affected finger. During this diagnostic delay, the proximal part of the ruptured tendon is likely to contract and curl up until surgical exploration. Though uncommon, the possibility of spontaneous closed intratendinous flexor rupture should be kept in mind when evaluating a patient who presents with a sudden inability to flex the interphalangeal joint in absence of open wounds.
Notes
Hyonsurk Kim is an editorial board member and Editor-inChief of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.