Minimal Incision Venectomy for Peripheral Septic Thrombophlebitis
Article information
Abstract
Peripheral septic thrombophlebitis is an uncommon but potentially lethal condition fraught with systemic complications. Optimal treatment calls for surgical excision of the inflamed venous segment, followed by antimicrobial therapy. However, the extended skin incision and meticulous flap elevation of conventional venectomy leaves substantial residual scarring. Herein, we detail a minimal incision venectomy performed for peripheral septic thrombophlebitis in a 55-year-old man. The patient was initially admitted for conservative management of intracranial hemorrhage but subsequently developed high fever and hypotension. An abscessed intravenous catheter site of the left forearm was the apparent source. Following emergency drainage and serial irrigation, surgical venectomy was undertaken to radically remove the septic focus, excising a 10-cm segment of infected vein through a separate proximal incision. After the procedure, the patient’s recovery was complete and free of complications at postoperative 6-month visit. Under appropriate indications, minimal incision venectomy can be an effective therapeutic alternative with minimal scarring.
Introduction
Septic thrombophlebitis is a life-threatening complication of venous infusion therapy resulting in high-grade and persistent bacteremia [1]. Central or peripheral veins may be involved, although cases linked to peripheral intravenous catheters have received less attention than those in which central catheters are implicated [2]. Often culminating in infectious hematogenous dissemination, peripheral septic thrombophlebitis accounts for a sizeable proportion of patients with potentially lethal septic thrombophlebitis [3].
Surgical excision of the inflamed venous segment, followed by antimicrobial therapy, is widely acknowledged as optimal treatment for septic thrombophlebitis [4]. Unfortunately, there are few reports documenting such surgical procedures, and the inevitable result of therapeutically successful venectomy is a lengthy scar marking the venous tract. Herein, we detail an instance in which peripheral septic thrombophlebitis was successfully treated with minimal incision venectomy. Existing publications on surgical treatment of septic thrombophlebitis are also reviewed.
This study was performed in accordance with the principles of the Declaration of Helsinki. The patient provided written informed consent for the publication and the use of his images.
Case
The patient was a 55-year-old man with no known underlying diseases. He, complaining of sudden dizziness in the morning, was diagnosed with intracranial hemorrhage of the right basal ganglia in his local hospital. He was transferred to our neurosurgical intensive care unit (NICU) for blood pressure control and antiepileptic medication. As vital signs were stable during NICU management for 5 days, he was transferred to the general ward.
His left cephalic vein was cannulated with a peripheral intravenous catheter by an intravenous injection team member. Two days following catheter change, the patient’s condition abruptly deteriorated. He developed high fever (up to 39.2°C), sweats, and rigors, with hypotension (Fig. 1). Cultures (blood, urine, and sputum) and computed tomography studies of chest and abdomen were obtained. However, only blood cultures yielded positive results and other culpable sources were not apparent. Intravenous empirical antibiotics (piperacillin/tazobactam) and inotropics (Norpin) were instituted, after which the patient was transferred to the medical intensive care unit.
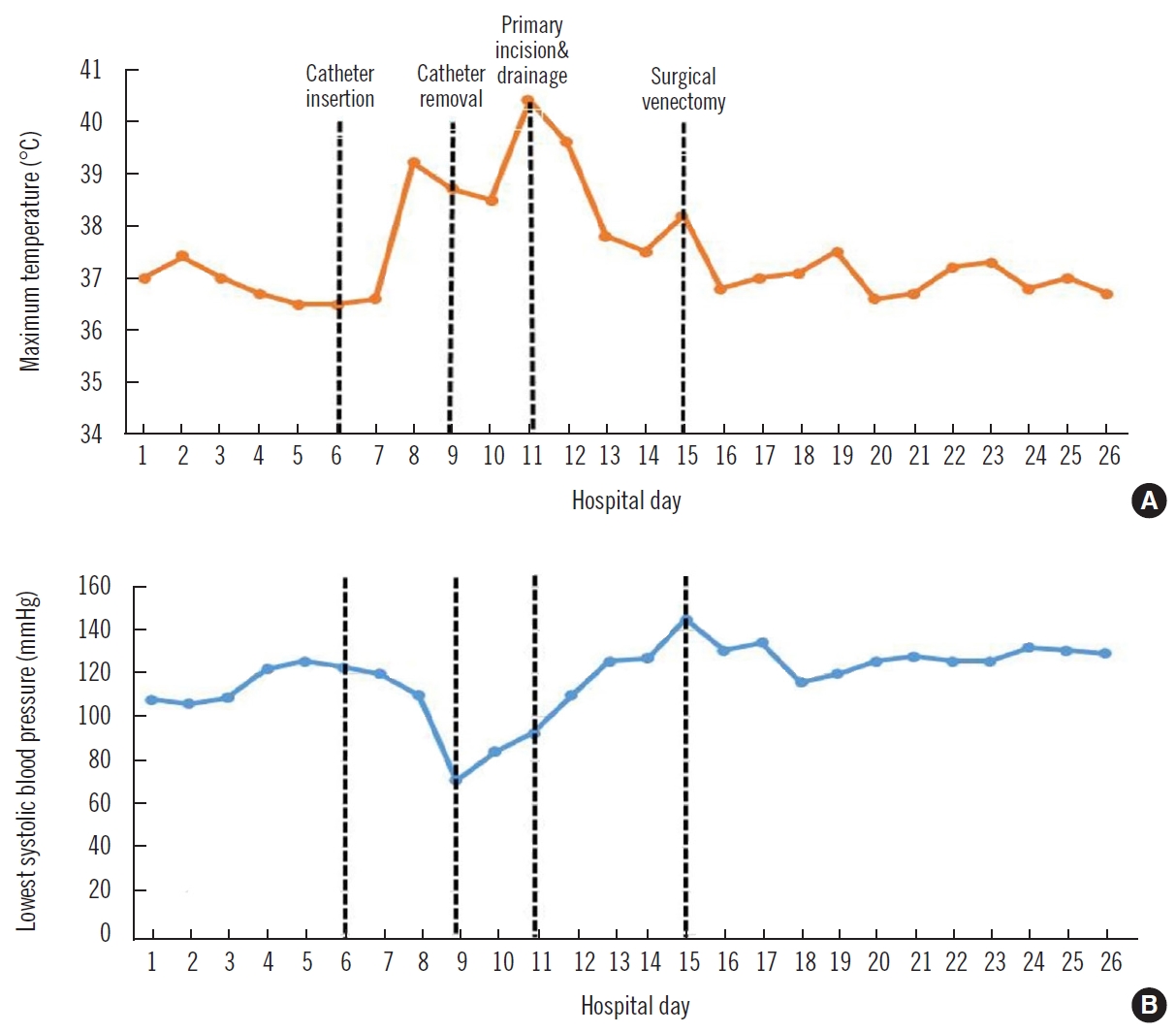
Clinical course of patient. Temperature (A) and blood pressure (B) demonstrated significant responses following procedures.
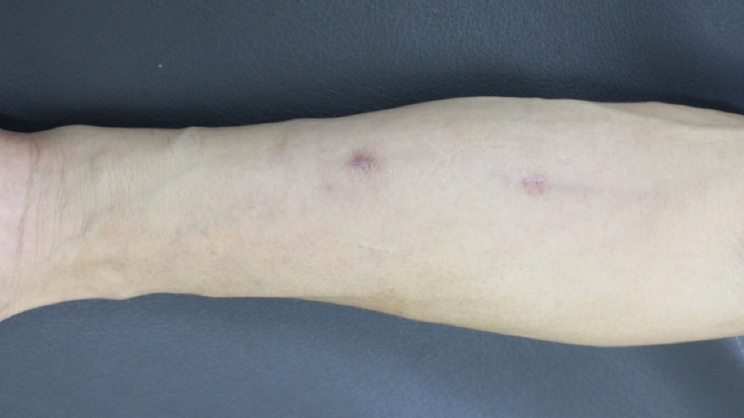
Tenderness and erythema of the cannulated left forearm were noted the day after his temperature spiked. The catheter was removed immediately and an initial regimen of arm elevation with warm compresses was performed. As prior blood cultures were positive for Citrobacter sp. and Enterobacter cloacae, the physicians changed the antibiotics to vancomycin and meropenem. The followed catheter tip culture showed growth of E. cloacae and Klebsiella oxytoca, and therefore antibiotics were changed to piperacillin/tazobactam and vancomycin. Despite appropriate intravenous antibiotics, erythema progressed along the vein and an abscess formed at the insertion site after 2 days from the catheter removal (Fig. 2). White blood cell count (range, 15,000–18,000/μL) and C-reactive protein level (24.2 mg/dL) were markedly elevated. Blood urea nitrogen and serum creatinine levels peaked at 36.4 mg/dL and 2.21 mg/dL, respectively.

Clinical photograph of patient with peripheral septic thrombophlebitis. An abscess formed at the intravenous catheter insertion site at left forearm and erythema progressed along the vein course.
We were asked for consultation around that time, and emergent incision and drainage were performed at bedside. A 2-cm-sized abscess was localized around the previous insertion site and the erythema with relatively clear margins spread to the proximal forearm along the vein course. The abscess mound was incised, releasing 3 mL of pus; a silastic drain was inserted to allow further drainage. Serial betadine irrigation was performed via silastic tube for 4 days removing necrotic detritus. Gradually, the blood pressure normalized, but fever persisted (up to 38.2°C).
Ultimately, venectomy was elected to radically excise the septic focus. The patient was taken to the operating room where a separate skin incision was made (proximal end of erythematous zone) under local anesthesia (Fig. 3). Below the incision, there was relatively loose space due to previous irrigation. The yellowish and thickened infected vein was found in the space and dissected from skin flap with sharp mosquito forceps. Once dissected and isolated, a 10-cm pus-filled segment was removed (Fig. 4). The uninvolved distal end was then ligated to prevent further bleeding. Culture of the surgical specimen again showed E. cloacae positivity, and in histologic preparations, there were intraluminal thrombus and necrotic detritus.

Postoperative photograph after minimal incision venectomy. Remote separate incision (black arrow) was made at proximal end of erythematous zone. Previous incision at abscess mound (white arrow) is shown.
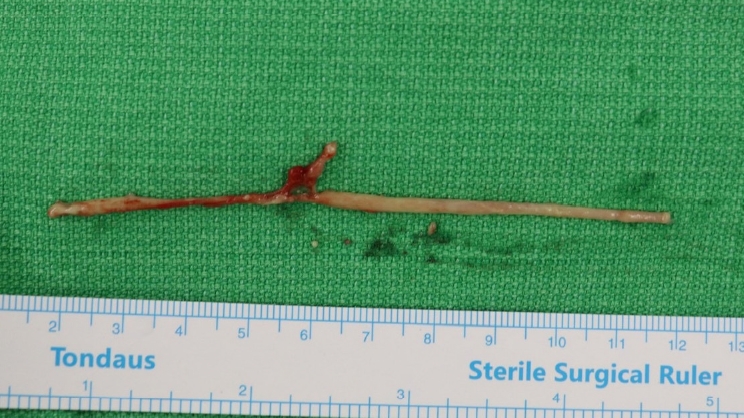
Excised specimen through minimal incision venectomy. A 10-cm sized yellowish and thickened infected vein was removed through a separate incision.
The patient’s recovery was quite dramatic. After the procedure, his fever promptly subsided, with normalization of both white blood cell and C-reactive protein in the course of 3 days. Swelling and redness of the left forearm also improved noticeably. He was discharged 11 days postoperatively on oral antibiotics and demonstrated complete wound healing after 2 weeks. At the 6-month postoperative follow-up visit, there was no evidence of recurrence or wound-related complication, with minimal scar formation (Fig. 5).
Discussion
Septic thrombophlebitis is a potentially lethal condition characterized by microabscess formation within a cannulated vein and repeated circulatory bacterial embolization [5]. Although steadily increasing in prevalence since the 1970s due to growing use of polyethylene intravenous catheters [2], its incidence is now declining thanks to the reduced durations of intravenous cannulation that past studies have underscored [6]. Broader usage of central vein cannulas may have further contributed to the drop in overall incidence, given the high flow and large caliber of these vessels [3]. Once developed, however, septic thrombophlebitis may become life-threatening, making early diagnosis and proper treatment essential.
Septic thrombophlebitis may be signaled by local symptoms, such as erythema, edema, abscess formation, and a palpably detectable cord. Still, half of such patients have shown a distinct delay between disease onset and diagnosis, because signs and symptoms may not appear for days [2]. A high index of suspicion is important in patients with persistent bacteremia or fungemia of unidentified sources [1]. The diagnosis relies on positive microbial cultures of blood and extracted catheters or demonstration of a thrombus by radiographic imaging [1,7]. Expression of pus from an exit site or purulent aspirate from a thrombosed peripheral vein is immediate confirmation of infection [4].
Infected veins should be surgically explored within 24–48 hours if prompt relief is not achieved by removing the tainted cannula and delivering appropriate antibiotic therapy [5]. Surgical intervention in this setting may include incision and drainage of an existing abscess, percutaneous mechanical thrombectomy, venous ligation, and resection of a thrombosed venous segment [2,8]. As in our patient, incision and drainage of a contiguous abscess is apt to immediately reduce fever, falling short of complete defervescence. An infected vein left in place is often associated with therapeutic failure [9]. Some authors advocate venous ligation, which does not seem viable for large central veins [9] and does not remove the septic focus, allowing bacteremia to continue (distal to the ligature) via deep venous circulatory collaterals [2].
Peripheral septic thrombophlebitis is most effectively managed by resecting thrombosed venous segments at accessible sites. However, this calls for lengthy skin incisions along vessel paths and meticulous flap elevation to create sufficient operative exposure. Because skin and subcutaneous tissues are edematous, and adhesions between inflamed tissues may be substantial, the process of flap elevation is prone to bleeding or flap congestion. In addition, high visibility of residual surgical scars is likely upon resolution.
In this case, we were able to remove the infected vein through a remote minimal skin incision. Early primary drainage and serial irrigation served to remove debris and limit inflammation, thus mitigating tissue edema and the propensity for adhesions. Therefore, inflamed veins could be easily removed because the subsequent tissue attachments were loose and easily disrupted by traction, without a subcutaneous flap for access. This method does not apply to deeply seated or central septic thrombophlebitis and is ill-advised if cutaneous erythema is not yet clear. However, minimal incision venectomy may be an effective therapeutic alternative when appropriate indications and preparation are made as follows: (1) early primary incision and drainage with serial irrigation; (2) distal and superficial catheter insertion site (cephalic or basilic vein distal to elbow crease); (3) erythema in short areas with clear margin; or (4) well-localized abscess along the vein course.
In conclusion, peripheral septic thrombophlebitis is a potentially lethal condition requiring proper surgical intervention and antimicrobial therapy. The extensive operative access of conventional venectomy leaves prominent scars, whereas minimal incision venectomy can be a quite effective alternative with minimal scars.
Notes
No potential conflict of interest relevant to this article was reported.