Sensate Neurovascular Island Flap for Thumb Reconstruction
Article information
Abstract
Thumb pulp defects require adequate reconstruction for satisfactory sensate function and aesthetic appearance. We report a reconstructive case using a sensate neurovascular island flap raised from the ulnar side of the middle finger for a tactile thumb pad defect. The flap was elevated as a modified version of the conventional heterodigital neurovascular island flap in order to restore thumb sensation without the “double-sensibility” phenomenon. The ulnar digital nerve of the flap was sectioned at the middle phalanx level of the donor digit and coaptated to the ulnar and radial digital nerves of the thumb through end-to-side and end-to-end neurorrhaphy. The remaining radial digital nerve of the donor finger was preserved, and the proximal end of the sectioned nerve was coaptated end-to-side to the radial digital nerve to prevent neuroma formation. No postoperative complications including venous congestion were observed. This technique is a relatively simple and reliable option for reconstructing thump pulp defects.
Introduction
Loss of the thumb results in significant functional and esthetic impairment; thumb reconstruction aims to restore movement, sensory function, length, and appearance. Among efforts to restore function and appearance in thumb amputation patients, replantation is the most commonly recommended surgical treatment. When replantation of the amputated segment is not possible, there are other reconstructive options such as skin grafting, or local, distal and free flaps. The treatment choice is usually guided by the level and extent of the injury. In wounds with exposed bone or tendon, flap reconstructions, instead of secondary healing or skin grafting, are usually the procedure of choice [1].
Different types of neurovascular flaps are suitable for sensory reconstruction under different conditions. While the neurovascular volar advancement flap is a useful reconstructive technique, it is limited to small volar and tip defects. Free sensate flaps harvested from various regions such as the thenar, hypothenar, and flexor aspects of the wrist are good options for larger defects. Recently, new techniques, including toe-to-thumb and wrap-around flap, have been widely applied. However, the free microvascular flaps are sometimes limited in application because of the extended operation time, greater skill requirements, and donor site morbidity [1].
The neurovascular island pedicle flap has been found to be a reliable technique for thumb-pulp reconstruction. In 1953, Littler [2] first demonstrated the island flap harvested from the medial side of the third or fourth finger for the thumb. The island flap provides one-stage reconstruction with adequate tissue of similar morphology and durable fasciocutaneous structures. In addition, the procedure is relatively easy and safe, requiring shorter operation time and a single operation field.
However, flap complications include venous congestion, scar contracture, numbness, cold intolerance, and hyperesthesia. In particular, failure of the sensory switching between the donor and the recipient or “double sensibility” of the flap can be a worrisome clinical problem after surgery. To resolve this concern, many modified versions of the neurovascular island flap were suggested. Several surgeons demonstrated the “disconnecting-reconnecting” technique by cutting the nerve within the flap and coaptating it to the proper digital nerve (PDN) of the thumb [3,4].
This article reports a case in which a sensate island flap was raised from the medial side of the third finger for thumb reconstruction. The donor ulnar PDN was divided at the middle phalanx and the proximal portion was preserved to minimize donor morbidity. Sensory nerve coaptations were performed to the radial and ulnar PDNs of the thumb to eliminate double sensibility and prevent neuroma formation. The study was performed in accordance with the principles of the Declaration of Helsinki. The patient consented to his images appearing in our publication.
Case
A 50-year-old male patient was referred to the clinic for an injury on his right thumb caused by a saw blade. He presented with soft tissue defect in the volar region of his right thumb (Fig. 1). According to the Allen classification, it was classified as type I without injured nail bed or distal phalangeal loss. After meticulous debridement, the size of the defect was found to be 2.3×3.5 cm. A relatively deep soft tissue defect with exposed bone and tendon was 1.0×1.5 cm, requiring flap coverage. Partial tear of the flexor pollicis longus tendon was repaired with 4-0 Ethibond. The distal ends of the ulnar and radial PDNs of the thumb were identified and prepared as recipient nerves.

Intraoperative photo showing the defect of the thumb pulp. The partially ruptured flexor pollicis longus tendon and distal phalanx base are exposed. There is no injury to the nail bed or distal phalanx.
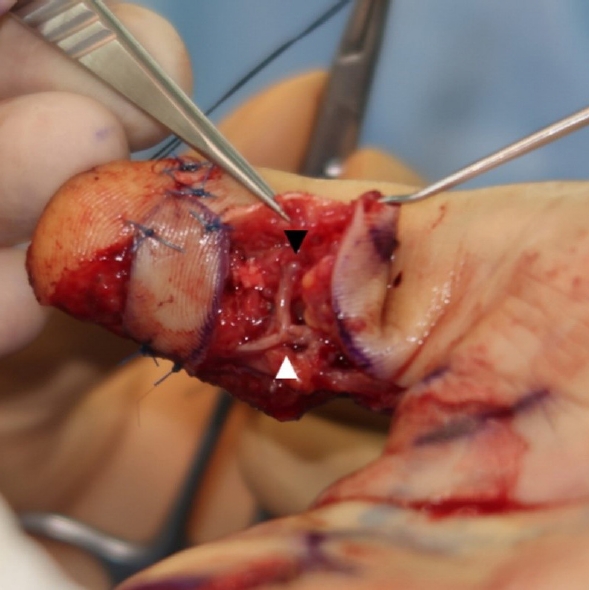
The flap was elevated from the ulnar side of the third finger following the original Littler technique [2]. Some surgical modifications were performed to improve sensation in the thumb and donor digit. The third ulnar PDN was involved in the flap and cut at the middle phalanx, leaving the remaining supply intact (Fig. 2). Careful dissection of the flap pedicle was done toward the proximal palmar crease. The fibro-fatty tissue around the neurovascular bundle was incorporated into the flap to allow venous drainage. The flap was then passed subcutaneously to the recipient site and fixed to cover the deepest tissue defect. The distal nerve ending that innervates the flap was connected with the radial and ulnar PDNs of the thumb in end-to-side and end-to-end fashions, respectively (Fig. 3). The proximal ulnar PDN at the donor site was sutured end-to-side to its lateral side to prevent potential neuroma formation (Fig. 4). All the nerve repairs were sutured using 9-0 nylon.

Intraoperative photo showing the flap elevation. Only the ulnar proper digital nerve is severed at the middle phalanx for anastomosis with the recipient nerve.

Recipient site view after transferring the island flap. The white triangle indicates the end-to-side anastomosis between the nerve innervating the flap and the ulnar digital nerve of the recipient. The black triangle indicates the end-to-end anastomosis with the radial digital nerve.
Donor site view after transfer of the island flap. The white triangle indicates the proximal ulnar digital nerve sutured end-to-side to prevent painful neuroma formation.
Finally, the glabrous skin of the amputated thumb was defatted and used to reconstruct the donor site of the third finger and the remnant skin defect of the distal thumb (Fig. 5). During flap dissection, the paratenon was preserved so that the skin graft could adhere. Additionally, split-thickness skin graft from the medial side of the upper arm was used for the remnant defect of the proximal thumb. The flap and graft survived well. There was no venous congestion observed in the transferred flap. The thumb pulp was successfully reconstructed with good color, texture and contour match. Tinel’s sign was positive in both thumb and donor finger at the 11-day follow-up. After a 6-month follow-up, satisfactory sensory recovery without double sensibility and pain was achieved on the reconstructed thumb. No other complications such as neuroma formation, hypertrophic scar, infection or hematoma were recorded. The patient was content with the aesthetic and functional outcomes of the thumb and the donor digit in performing daily activities at work or at home (Fig. 6).

Immediate postoperative photographs. (A-D) After the tourniquet is released, good blood supply without venous congestion (black triangle) is observed in the flap tip.
Discussion
The thumb pulp is critical for the pinch maneuver; when it is damaged, neurovascular flaps are preferred for their sensory reconstruction. Homodigital or heterodigital neurovascular island pedicle flaps provide a one-stage method for sensory reconstruction for the thumb pulp [1]. The Littler flap has the advantages of needing only a single operative field with shorter operation time. However, the classic procedure has several inherent disadvantages. In particular, the phenomenon of “double-sensibility” is a challenging clinical issue. This phenomenon has been attributed to insufficient cortical reorientation, which may persist despite multiple years of sensory re-education. Theoretically, the conventional technique may be suitable in children with a higher capacity to reorient. However, in most adults, especially those whose occupations require manual dexterity, this complication can cause patient dissatisfaction [5].
In order to address the issue, many studies have suggested surgical modifications. Foucher et al. reported that the nerve carried by the flap was anastomosed end-to-end with the sectioned PDN of the thumb to resolve the double-sensibility phenomenon. Their “disconnecting-reconnecting technique” included transecting PDN of the donor digit in the palm during flap elevation and coaptating it to PDN of the thumb in an end-to-end manner [3,6]. Adani et al. and Oka reported satisfactory results, with double-sensibility phenomenon not found in the modified procedure. The results were better with respect to paresthesia, pulp-writing test, as well as the switching phenomenon [4,5].
However, there remains the risk of sensory loss in the donor site. To minimize donor morbidity, Rose suggested the nerve-stripping technique–namely, microsurgical separating the digital nerve from the vascular pedicle to preserve donor sensibility [7]. While raising the flap, extreme care should be taken to prevent not only complete transection of PDN, but also injury to the fine venous system next to the digital artery. A cuff of the fibro-fatty tissue surrounding the neurovascular bundle should be incorporated for venous drainage. Venous congestion of the flap is a potential problem in the early postoperative period, but it does not compromise the overall flap viability [1,7]. In our case, PDN of the flap was cut to a minimal length that allowed tension-free neurorrhaphy to PDN of the thumb (Figs. 2, 3). The proximal portion of the donor finger’s PDN was carefully separated from the vascular pedicle of the flap and left intact. No congestion was observed in our case, but it is postulated that a larger flap size might increase the risk of venous congestion.
Preventing painful neuromas is another issue in the modified Littler flap. Some studies reported that the proximal end of PDN was embedded in the adjacent muscle, such as the lumbrical muscles of the palm [6] or the thenar muscle at the base of the thumb [4]. In our case, the proximal stump of PDN at the donor site was managed with end-to-side anastomosis to its lateral side (Fig. 4). The use of end-to-side neurorrhaphy is well established in surgical management and prevention of neuropathic pain arising from neuromas [8]. In addition, nerve coaptations at the recipient site can eliminate double sensibility, and decrease the risk of potential neuroma formation due to incomplete repair of the nerve ending following the injury. To the best of our knowledge, this is the first case wherein both the ulnar and radial PDNs of the thumb were coaptated to the single nerve of the island flap using end-to-side and end-to-end techniques (Fig. 3). Meanwhile, recent studies have shown modified Littler flap supplied by the dorsal branch of PDN and PDN from the ulnar aspect of the third finger [9,10]. The sensory nerves carried by the flap were repaired to the ulnar and radial PDN in the recipient, respectively.
Our case shows the utility of the modified neurovascular island pedicle flap as a sensate flap for thumb-pulp defect in a one-stage operation. Furthermore, we used microsurgical neurorrhaphy techniques to contribute to better sensation, and minimize the risk of neuromas at the donor and recipient sites.
Notes
No potential conflict of interest relevant to this article was reported.

