Hatchet Thigh Flap with Hemi-gluteus Flap for Recurrent Ischial Sore Reconstruction
Article information
Abstract
Background
Ischial pressure sores are the most challenging sores to treat because of associated bursa and high rate of recurrence. Reconstruction flaps originating in the thigh have a disadvantage as movement may increase shear forces, and tension during closure may lead to wound dehiscence. To circumvent these problems, we hereby present a hatchet thigh flap with good mobility, which can be used for recurrent cases as well.
Methods
All patients treated at our hospital in the last 5 years for ischial pressure sores were included in the study. The flap is elevated in the subfascial plane from lateral to medial until the medial circumflex artery perforators are revealed. In recurrent cases the lower half of the gluteus maximus muscle is used to fill in the cavity while the flap from the previous surgery is re-advanced.
Results
Sixteen patients (11 males and five females) were in the study. The median age of the patient was 54 years (range, 25–82 years). All the flaps survived fully. Two patients had recurrence at three sites, which were successfully reconstructed by advancing the same flap and hemi-gluteus muscle. An average of 6 months follow-up after surgery for recurrence showed stable reconstruction.
Conclusion
The hatchet thigh flap is easy to dissect and reliable for ischial pressure sores. It can be used effectively in recurrent cases when combined with hemi-gluteus flaps.
Introduction
Ischial pressure sores occur in paraplegic patients who remain chair-bound for long periods of time without changing their positions [1]. The sores usually have a small skin defect accompanied by deep tissue loss. The deep cavity at ischial tuberosity requires adequate padding for reconstruction. These are difficult to treat and have high risk of recurrence [2]. As patients with ischial sores often also have pressure ulcers in other locations, surgeries should be planned with care to prevent one surgery from disrupting another [3]. The reconstruction of ischial sores requires flaps from the gluteal region or posterior thigh [4]. The latter, originating from the thigh, is subject to shear forces with leg movement, and closure under tension [5]. We present here a hatchet-shaped posterior thigh flap for ischial pressure sore reconstruction with adequate mobility to obtain tension-free closure, with the added advantage of avoiding areas of reconstruction for other sores. In recurrent cases, this hatchet flap can be readvanced along with a muscle flap to obliterate the cavity.
Methods
In this retrospective study, patients who had visited the institution from March 2015 to March 2020 with grades 3 or 4 ischial pressures sores were included. The study included both new and recurrent cases. Patients with grades 1 or 2 ischial pressure sores were managed conservatively and were therefore excluded from the study. Patients lost to follow-up were also excluded from the study. Preoperative magnetic resonance imaging was performed to rule out osteomyelitis of the ischial tuberosity.
The operation is performed under general anesthesia in the prone jack-knife position with appropriate protective padding. The pressure ulcer is debrided thoroughly, taking healthy margins. This involves removal of all surrounding fibrotic structures and bursae. The ischial tuberosity is blunted conservatively and smoothened with a rasp.
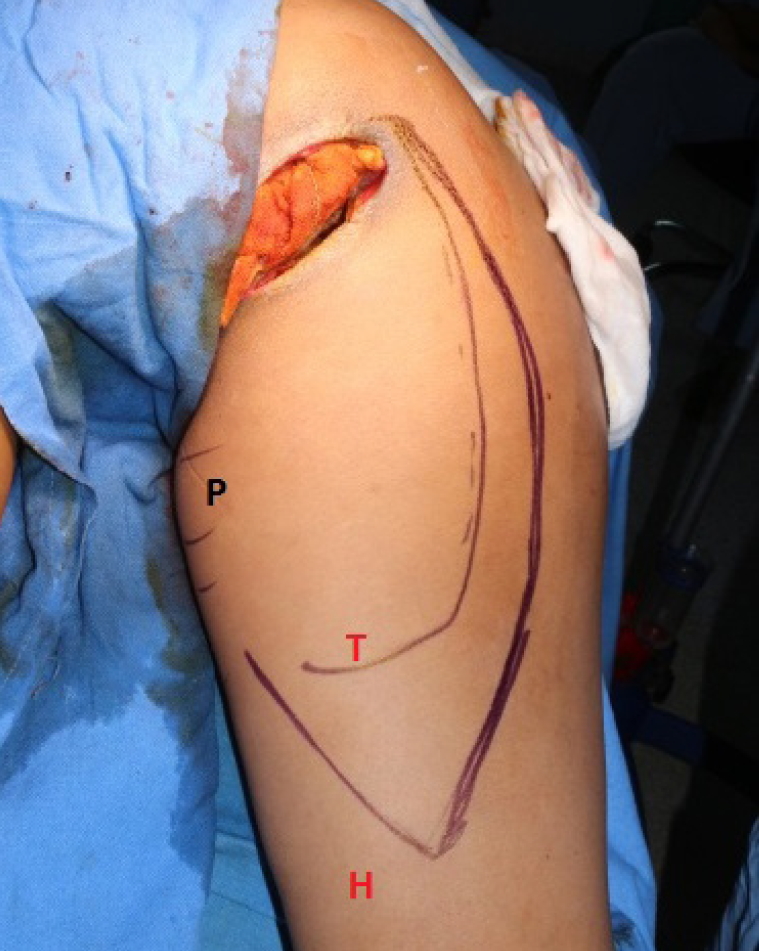
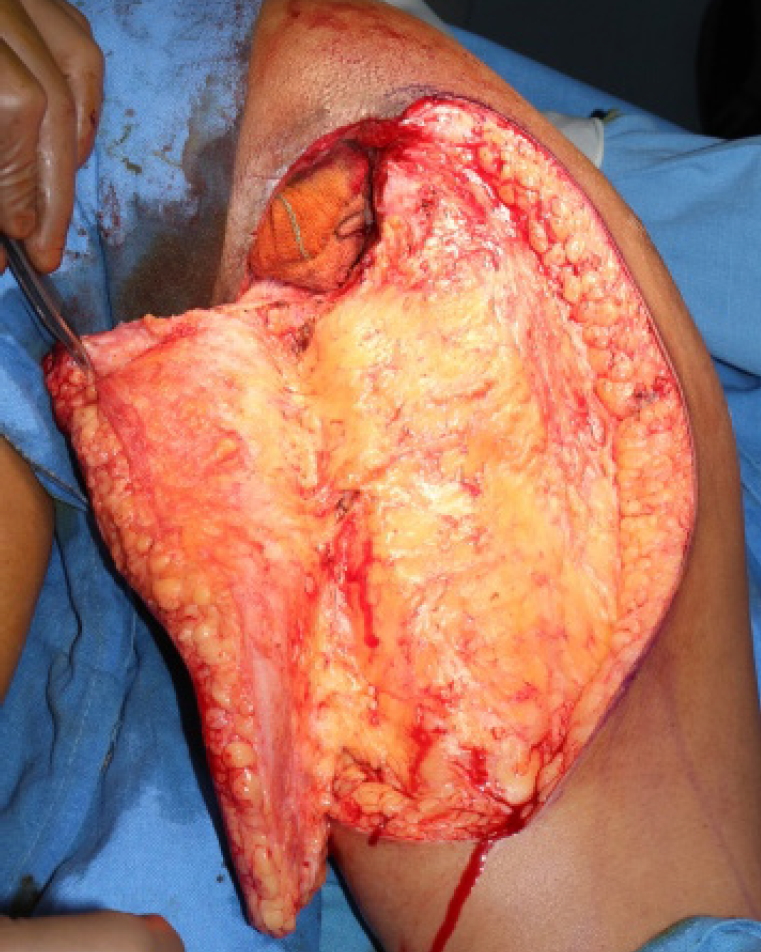
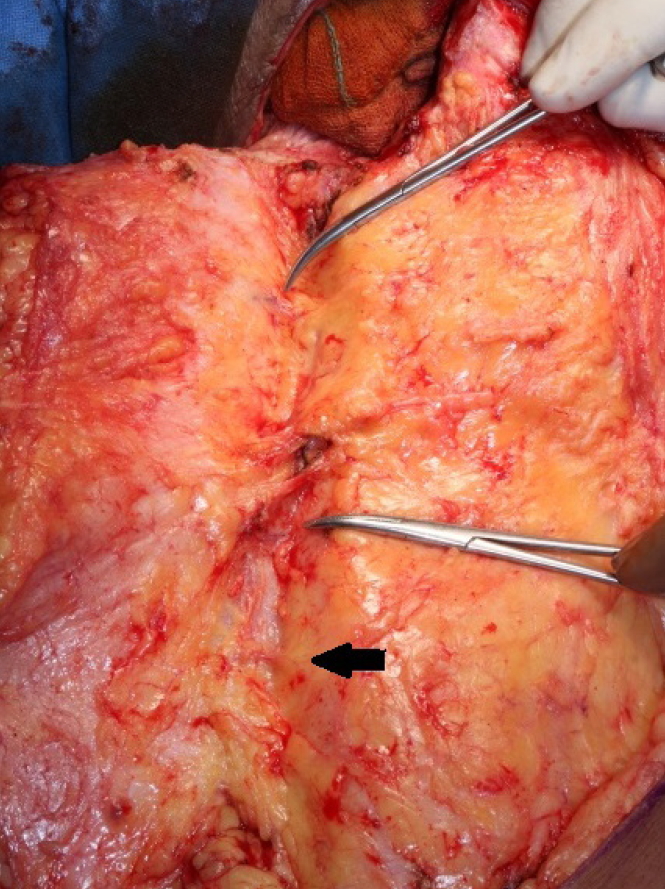
The hatchet flap is marked involving the upper two-thirds of the posterior thigh (Figs. 1, 2). The flap is elevated in the subfascial plane from lateral to medial (Fig. 3) until the medial circumflex artery perforators are revealed (Fig. 4). These perforators arise from the transverse branch of medial circumflex femoral artery. Two to three perforators are usually observed. The flap is adequately mobilized, especially in the area near the ulcer and distally near the back-cut area, to obtain sufficient mobility for the flap to reach and fill the defect. The part of the flap in contact with the ulcer is de-epithelized and turned inwards to provide additional bulk over the ischial tuberosity (Fig. 5). Closure is done in single layer using nylon sutures (Fig. 6). When the cavity is large (as in the case of a recurrent ulcer) and requires tissue for obliteration, a hemi-gluteus flap is used. The lower half of the muscle which lies in the wound just adjacent to the defect is mobilized by detaching its insertion to the greater trochanter. Gluteus maximus is the most superficial muscle of the gluteal region. The muscle fibers are cut along the direction of its fibers so that the muscle could be easily transposed to fill the defect. Antibiotics are continued for 2 weeks.
Postoperatively, patients are placed in supine bed rest on a low pressure mattress (Auto Logic; ArjoHuntleigh, Houghton Regis, UK) for 2 weeks. On postoperative day 15, they are transferred to a pneumatic ripple bed (Secura; Norma, New Delhi, India) and a limited sitting protocol, beginning with three 30-minute sittings a day, is initiated and overseen by the physical medicine and rehabilitation team. Informed written consents for the photographs were obtained for use in the journal.
Results
Eighteen flaps were taken for ischial pressure sores in 16 patients (11 males and five females) (Table 1). Most of the patients had spinal cord injuries leading to grades 3 and 4 ischial sores of varying durations, from 10 months to 10 years. The median age of the patient was 54.4 years (range, 25–82 years). Diabetes mellitus was the most common associated co-morbidity. None had osteomyelitis of ischial tuberosity. All the flaps survived fully. One patient developed a minor wound infection on postoperative day 6 but was managed with regular dressings. Two patients had recurrence. One patient with bilateral ischial sores had recurrence in both of the sores, but at different times. All the recurrences were managed with flap readvancement along with a hemi-gluteus flap. The wounds remained stable until the last follow-up averaging 6 months (range, 3–10 months) postoperative. Average duration of the hospital stays was 8 days (range, 3–17 days). All the patients were managed on antibiotics according to cultures and no special dressings were used postoperatively. Klebsiella was the most common microorganism isolated in the wounds.
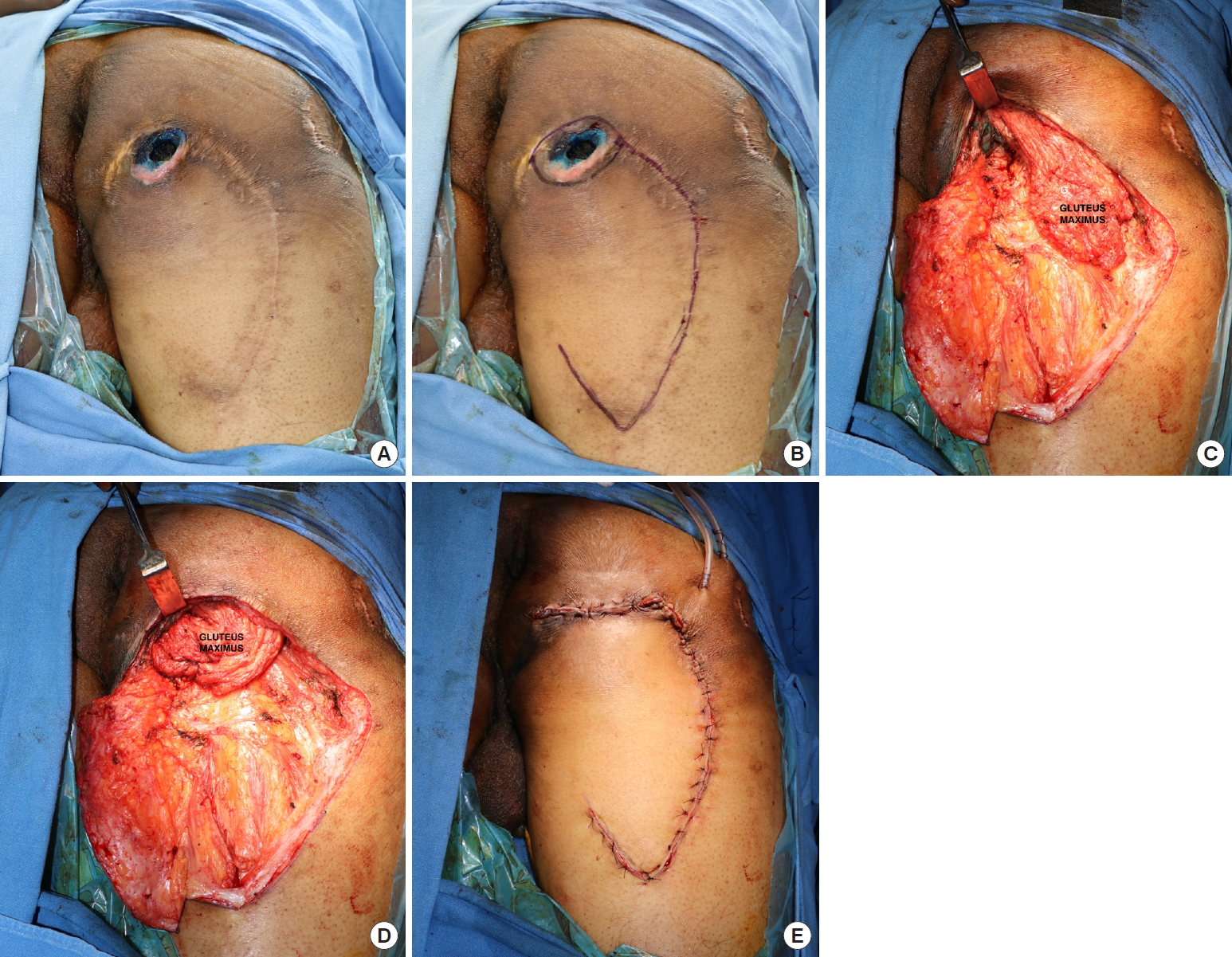
The patient of recurrent case, a 60-year-old male with an ischial sore after sustaining spinal cord injury, received debridement of the wound. He then had hatchet flap surgery and had a recurrence 1 year later (Fig. 7A). The wound was explored (Fig. 7B) using the hatchet flap from his earlier operation. The gluteus maximus muscle lay adjacent to the defect (Fig. 7C). A hemi-gluteal flap was transposed to obliterate the cavity (Fig. 7D), and the wound was closed by insetting the same flap (Fig. 7E).
Discussion
There are numerous flaps enlisted in literature for reconstruction of ischial pressure sores (Table 2) [5]. An ideal flap used for pressure sores should have reliable blood supply, be bulky enough to cushion the bony prominence, should not hinder the use of other flaps and preferably should not leave a secondary defect that needs to be covered with a skin graft [6].
Depending on the composition, flaps for ischial sore coverage can be muscle/musculocutaneous flaps, fasciocutaneous flaps, perforator flaps or combinations of the above. Muscle flaps have the advantage of better filling the cavity and enhanced clearance of bacteria. However, they are less tolerant of ischemia when subjected to pressure again, and furthermore, donor morbidity is of concern in non-paraplegic patients [7]. As for fasciocutaneous flaps, they cover the bony prominence better and are easy to dissect. These can also be re-advanced in case of recurrence. Meanwhile, perforator flaps have the advantage of longer pedicles for flap advancement and can be moved with ease. However, perforator flaps are more difficult to dissect and are more prone to venous congestion [8]. Dissection of islanded perforator flaps is difficult to learn and hence is performed by more experienced surgeons.
Fasciocutaneous flaps from the posterior thigh area have been used for ischial sore management mostly as transposition flaps [6]. The problem of using these as transposition flaps is that they cannot be re-advanced in case of recurrence, whereas hatchetshaped flaps can be used for new as well as recurrent cases.
Early recurrence of the ulcer occurs due to either inadequate excision of the bursa or inadequate filling of the soft tissue. Late recurrence is usually because of the patient’s non-compliance. For a large and deep cavity, a perforator/fasciocutaneous flap along with a muscle is ideal, as the muscle fills the dead space and is better able to stand the test of time [9]. Various combinations of muscle flaps with fasciocutaneous/perforator flaps are enumerated in literature for recurrent ulcers, such as the gluteus maximus muscle [9], medial circumflex artery flap with biceps femoris [6], gracilis and V-Y profunda femoris artery flap, and profunda artery flap with biceps femoris [10]. We used the hatchet thigh flap with hemi-gluteus muscle for recurrent cases, yielding good results with no recurrence for an average follow-up of 6 months.
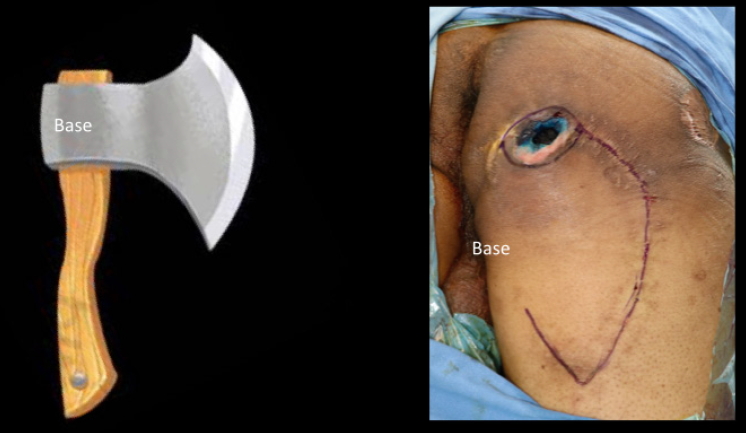
The hatchet flap, dubbed so because it resembles the blade of a hatchet, a small axe with a blade that narrows where the handle is fastened, also has a narrow base that increases its freedom of movement. If the flap is planned so that there are perforators in the base, the vascularity of flap and its reach could be enhanced (Fig. 8). The hatchet flap is commonly used where the donor site is closed primarily in a V-Y fashion. The surrounding skin is incorporated to cover the defect. It is extensively used for reconstruction of defects and can be easily re-advanced [11]. One disadvantage of the hatchet flap is its limited mobility as compared to perforator flaps as the blood supply of the hatchet flap comes from the base of the flap. In case of the need for extensive mobilization, islanded perforator flaps should be the method of choice.
For reconstruction of ischial sores, we present here a reliable hatchet flap from the posterior thigh, which allows for easy dissection, and can be re-advanced in case of recurrence along with hemi-gluteus muscle without extending the incision to new areas. Given the ease of the dissection of this method, it may be employed by less experienced surgeons as well.
The limitation of our study is that it is a retrospective analysis. Long-term results of recurrent sore management should be assessed in a large multicentric study to demonstrate consistent results in recurrent ischial sores.
In conclusion, the hatchet thigh flap is an easy-to-dissect, reliable flap for ischial pressure sores. This flap can be effectively utilized along with hemi-gluteus muscle for recurrent sores.
Notes
No potential conflict of interest relevant to this article was reported.