Causes of Surgical Wound Dehiscence: A Multicenter Study
Article information
Abstract
Surgical wound dehiscence is a postoperative complication involving breakdown of surgical incision site. Despite the increased knowledge of wound healing mechanism before and after surgery, wound dehiscence may increase the length of hospital stay, increase patient inconvenience and rates of re-operation. The purpose of this study was to analyze the causes of wound dehiscence in patients undergoing reoperation at 4 hospitals of Soonchunhyang Medical Center. The number of patients in each hospital and those operated previously were compared. In addition, other characteristics of patients were compared in patients who underwent reoperation. In 22 out of 1,026 patients consulted at the Seoul hospital, 32 cases out of 1,295 at Bucheon hospital, 14 cases out of 1,687 at Cheonan hospital and 15 cases out of 374 at Gumi hospital, wound revision was performed for wound dehiscence. Patients at the Department of Obstetrics and Gynecology were the most common and included 33 patients (39.8%). The most common intervention before wound revision was Cesarean section in 14 patients (19.3%). In this study, we retrospectively reviewed patients who underwent wound revision due to wound dehiscence and analyzed the underlying causes of the postoperative complication.
Introduction
Surgical wound dehiscence is a postoperative complication involving breakdown of surgical incision site. Despite the increased knowledge of wound healing process before and after surgery and the development of preoperative care and suture materials, wound dehiscence may increase the length of hospital stay, increase patient inconvenience and rates of re-operation. In addition, wound dehiscence after abdominal surgery is associated with mortality rates of 10−44% [1,2].
Several studies investigated risk factors causing wound dehiscence. Patients older than 65 years are more likely to develop wound dehiscence because of deterioration in tissue repair mechanism compared with younger patients [3]. Other well-known risk factors include hypoproteinemia, local wound infection, anemia, hypertension, and emergency surgery [1]. Risk factors that increase intra-abdominal pressure such as abdominal distension, excessive coughing, vomiting, and constipation increase the possibility of wound dehiscence after surgery [4]. In addition, surgical experience, operative time exceeding 2.5 hours, type of incision, suture material, drain, medical history such as obesity with body mass index (BMI) greater than 30 [5], stroke, chronic obstructive pulmonary disease (COPD), pneumonia, and malignancy also affect wound dehiscence [6]. In particular, studies show increased wound dehiscence rates in patients with more than 5 risk factors [1].
Despite many studies investigating the risk factors causing wound dehiscence and efforts to control them, patients continue to suffer from wound dehiscence. The purpose of this study is to analyze the causes of wound dehiscence in patients undergoing reoperation at 4 hospitals of Soonchunhyang Medical Center, South Korea.
Methods
From January 2013 to November 2017, patients underwent surgery at other departments and reoperation following a diagnosis of wound dehiscence and referral to the Department of Plastic and Reconstructive Surgery at 4 hospitals of Soonchunhyang Medical Center. The patients were divided into two groups: conservative treatment and surgical treatment. The number of patients in each hospital and previous operation were compared. In addition, age, time from previous surgery to postoperative reoperation, and other medical histories were compared in patients who underwent reoperation.
Results
Twenty-two out of 1,026 patients consulted at Seoul hospital, 32 cases out of 1,295 at Bucheon hospital, 14 cases out of 1,687 at Cheonan hospital and 15 cases out of 374 in Gumi hospital, underwent wound revision for wound dehiscence (Table 1). The patients were classified according to age, previous diagnosis or operation, duration of revision after first operation, and past medical history (Table 2). The patients included 27 males (32.5%) and 56 females (67.5%) with an average age of 48.35 years (0–89 years). Obstetrics and Gynecology (OBGY) was the most common department with 33 patients (39.8%) followed by 15 patients from Neurosurgery (NS), 11 patients from Orthopedic Surgery (OS), 10 patients from General surgery (GS), 8 patients from Emergency Medicine (EM), 2 patients from Thoracic Surgery (TS), 2 patients from Internal medicine (IM), 1 patient from Urology (UR), and 1 patient from Otolaryngology (ENT) departments. The most common surgical history was primary repair by various departments (16 patients, 19.3%). The second common surgical history was Cesarean section (C/Sec) in 14 patients (16.9%), which accounted for 42.4% of all patients who underwent wound revision after operation at OBGY. The mean BMI of the patients was 24.4 (Range of 15.97−45.26). The mean BMI of the patients of OBGY was 25.98 (Range of 18.59−45.26), and patients who underwent C/Sec was 24.73 (Range of 19.75−29.2). Nineteen patients (22.9%) had a history of hypertension (HTN) and 10 patients (12.0%) had diabetes (DM). The current or ex-smokers included 15 patients (18.1%) and the average pack-year (PY) was 15.3 PYs (Table 3). The mean time from the first operation to wound revision was 30.8 days. It was 24.29 days for patients from OBGY and 25.98 days for patients undergoing C/Sec was.
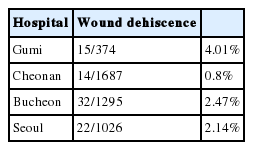
Comparison of patients referred to Department of Plastic and Reconstructive Surgery and patients who underwent wound revision for wound dehiscence at four hospitals of Soonchunhyang Medical Center

Characteristics of patients who underwent wound revision at Department of Plastic and Reconstructive Surgery at four hospitals of Soonchunhyang Medical Center
Discussion
Various causes of wound dehiscence include surgical experience, surgical incision, suture material, and patient factors such as age, nutritional status, and other accompanying diseases [1,4–6]. Preoperative risk factors include poor laboratory findings, infection, hypertension, and emergency surgery [1]. In particular, wound infection is the most relevant factor [6], and it increases the possibility of wound dehiscence by decreasing tensile strength and fibroblast concentration. Decreased fibroblast concentration triggers tissue destruction during wound healing [1]. Hypoproteinemia also reduces tensile strength [6]. It is required to reduce the incidence of wound dehiscence through preoperative control of these areas. Postoperative risk factors include abdominal distension, excessive coughing, vomiting, and constipation [5], and resolving these symptoms with appropriate medication may reduce the likelihood of wound dehiscence
In this study, we retrospectively reviewed patients who underwent wound revision due to wound dehiscence with reference to various causes. We reviewed the operative and other medical history prior to wound revision and analyzed the causes of wound dehiscence.
First of all, proportion of female patients were higher than male patients, but this result may be less meaningful in that proportion of patients with wound dehiscence was higher in OBGY patients. The most common surgical history was primary repair, but this also has less significance in that this data includes primary repair in the emergency room by residents. Unlike previous literature, age, BMI, medical or social history did not show any special significance in this study. However, The results suggest that the proportion of patients with wound dehiscence requiring wound revision was higher in patients who underwent operation by OBGY department, especially after C/Sec. This high rate of wound dehiscence after C/Sec or other OBGY surgery at multiple center of this study suggest that there may be some relation between wound dehiscence and OBGY surgery, especially C/Sec.
C/Sec is still one of the most commonly used surgical techniques in obstetrics and gynecology. Currently, 36% of deliveries in Korea are performed by C/Sec [7]. In the United States, about one-third of all mothers undergo C/Sec, and 15% of all deliveries worldwide are performed by C/Sec [8]. Despite the generalization of C/sec, marital morbidity and mortality risk are still higher than vaginal delivery [5,8]. Wound dehiscence and infection after C/Sec are important causes of postoperative morbidity and account for 10% of pregnancy-related mortality [10]. The rate of postoperative wound dehiscence after C/Sec has been reported to be 2.5−16% [11]. In this study, 16.9% of patients who underwent wound revision were C/Sec patients despite the usual method, which shows that our results are similar to those of previous literature. On the other hand, the rate of wound dehiscence after other abdominal surgery has been reported to be 0.4−3.5% [2,3,6], However, there are few studies comparing C/Sec or OBGY surgery with other abdominal surgery.
In addition, previous studies have shown that wound dehiscence usually occurs 4 to 14 days after surgery and occurs most commonly between 6 and 8 days. Wound dehiscence may occur even after 30 days post-surgery [2,4]. In this study, wound revision was performed at an average of 30.8 days after the first operation. However, one limitation of our data is that the actual onset time of wound dehiscence was not verified; there probably will be some difference between the onset of dehiscence and the time of re-operation.
The limitations of this study are as follows: First, the number of patients is limited, and the effect of other factors may not be considered as a retrospective study. Second, when selecting the patient group, the patient’s diagnosis was retrospectively confirmed. Therefore, it is possible that these patients may have been excluded in the absence of a diagnosis of wound dehiscence although wound revision was performed. Third, because of the selection of patients who underwent wound revision among patients with wound dehiscence, the boundary between surgery and conservative treatment was based on subjective aspects. Fourth, other aspects of the patient group were not considered. For example, severe abdominal distention results in a higher incidence of wound dehiscence [1]. However, the factors for evaluation of maternal abdominal distension were not reflected in the patients who underwent C/Sec.
This study showed a difference in wound dehiscence based on the type of surgery. A randomized controlled study with large number of patients undergoing different surgeries and collaborative research among multiple departments is needed. Such a study will facilitate identification of modifiable risk factors for surgery with a high probability of wound dehiscence and focus attention on the control of risk factors contributing to wound dehiscence.
Conclusion
This study analyzed the incidence of surgical wound dehiscence by investigating the causative factors and the differences among patient groups across several medical centers. Therefore, it is essential to consider the risk factors causing wound dehiscence in advance for preventive interventions. In addition, further studies with a well-controlled and cooperative design are required to address the study limitations.
Acknowledgements
This work was supported in part by the Soonchunhyang University Research Fund. No potential conflict of interest relevant to this article was reported.
