Introduction
Rosai-Dorfman disease (RDD) is a rare histiocytic disorder that typically presents with lymph node invasion; less than 1,000 patients have been reported since it was first described in 1965. Purely cutaneous RDD, which only presents cutaneous symptoms, is regarded as a separate disease entity, as it has a different progression and epi-demiology, and is even rarer than classical RDD. Cutaneous RDD occurs at the average age of 43.5 years and is more frequent in Asians and Caucasians. In addition, the number of female patients is twice that of male patients. In contrast, classical RDD occurs more commonly in Africans, with an average onset age of 20.6 years. Classical RDD occurs 1.4 times more often in males than in females [1].
RDD mainly presents lymphadenopathy accompanied with night sweats, fever and weight loss, but it also can show cutaneous extranodal symptoms. Herein, we present a case of a female Korean patient who presented a chronic skin ulcer and was finally diagnosed with RDD. The study was approved by the Institutional Review Board of Inje University Haeundae Paik Hospital (IRB No. 2022-07-011). The patient provided written informed consent for the publication and use of her images.
Case
A 55-year-old woman visited our plastic surgery outpatient clinic with a 1×1 cm nodule on her left cheek. She first noticed it a month prior to presentation without any history of trauma, infection, or insect bites. The skin nodule was palpable and nontender. It had a round shape showing skin dimpling around its margin. It gradually increased in size and had yellowish discharge coming out from its central hole. The nodule was ini-tially suspected to be an inflamed epidermal cyst. There were no specific abnormal findings in the blood tests, including complete blood count, electrolyte levels, and liver profile. An excisional biopsy was performed, and the pathology results in-dicated inflamed granulation tissue with infiltration of inflammatory cells (Fig. 1).
Fig. 1.
Photograph of a 1×1-cm nodule on the patient's left cheek. (A) Preoperative image of a skin nodule resembling an epidermal cyst. (B) Histological section displaying granulation tissue with a numerous infiltrating inflammatory cells (H&E stain, ×100).

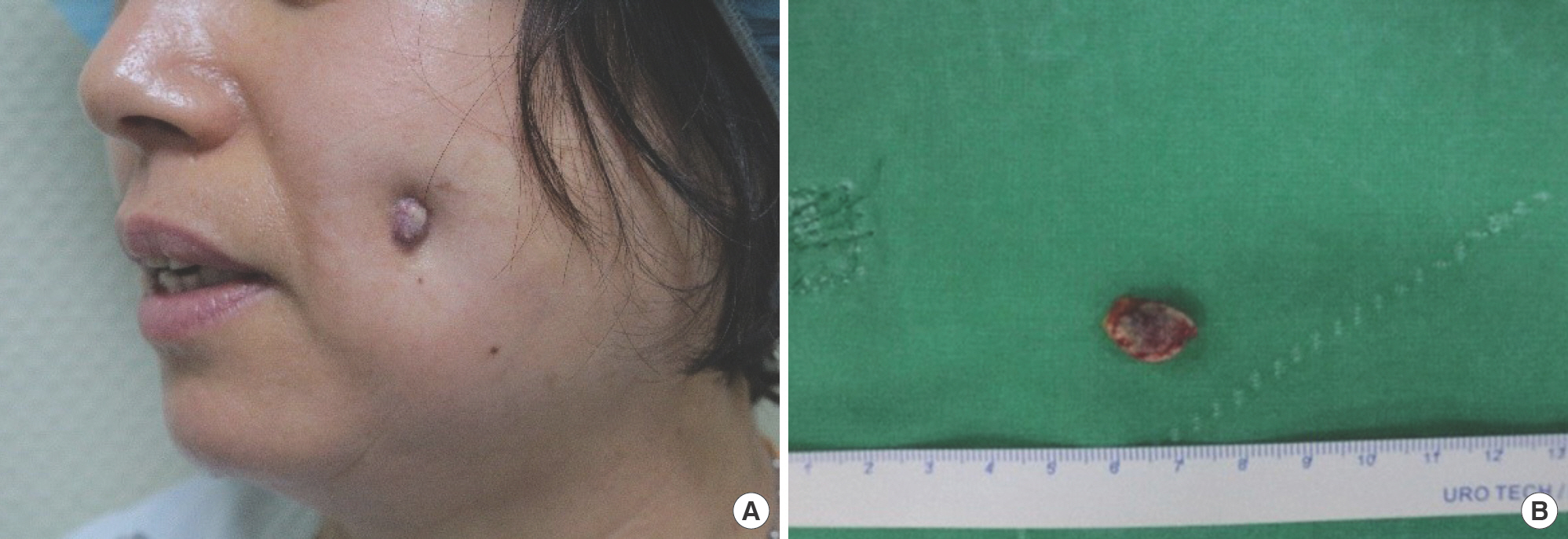
In the first postoperative month, the excision site healed well without any complications. However, 1 month later, a skin lesion recurred at the same site. An ulcer formed on the surface with yellowish discharge. Repetitive simple dressings along with oral antibiotics (cefpodoxime 100 mg twice daily) were administered for 3 months in the outpatient clinic. At first, the wound seemed to improve but soon it progressed and a nodule of approximately 1×1 cm was formed. Clinically, we diagnosed it as a recurrence of the epidermal cyst. Hence, under local anesthesia, we performed wide excision with a margin of about 3 mm, and curettage on the wound bed to prevent an-other recurrence (Fig. 2).
Fig. 2.
Ulcerative skin nodule on the previous excision site. (A) The photo was taken 1 month after the initial excision. An ulcerative nodule recurred at the excision site. (B) Photograph of an excised specimen about 1×1 cm in size.
Biopsy of the secondarily excised lesion revealed previously undiscovered findings. It showed a collection of histiocytes in the dermis with cytoplasm engulfing other inflammatory cells, matching the description of emperipolesis. Immunohisto-chemical analysis displayed positive staining of the histiocytes for S-100 proteins and CD68 proteins. However, they were not stained with periodic acid-Schiff staining with diastase, indi-cating RDD (Fig. 3).
Fig. 3.
Histological and immunochemistry findings of the specimen. Histology results are shown in this photo. Each section is stained in (A) periodic acid-Schiff staining with diastase (PAS-D), (B) S-100 protein, and (C) CD68. Histocytes were PAS-D negative, S-100 positive, and CD68 positive. All three images show the inflammatory cells engulfed by the cytoplasm of histiocytes (A and B, ×100; C, ×400).

The patient had no underlying diseases other than non-alcoholic fatty liver disease. She had undergone regular health check-ups, and the blood tests at her first visit with us were normal, making systemic diagnosis difficult. The results of the last biopsy were considered to indicate cutaneous RDD be-cause the patient did not have any other distinct symptoms. However, a thorough retrospective investigation revealed that the patient had repeatedly experienced cervical lymph node enlargement. Additionally, she sometimes experienced night sweats and fever, which she thought were inconsequential. Therefore, it was reasonable to regard the skin manifestations as extranodal symptoms of classical RDD.
After the last biopsy, the patient was followed-up monthly without supplementary treatment such as steroid therapy. There was no recurrence or any other complications for 6 months. The excision site healed well with satisfactory cosmetic results. Additionally, the patient underwent a chest and abdominopelvic computed tomography (CT) to rule out undiscovered lymph node or organ invasion; no specific invasion was found. However, RDD can commonly recur; hence, the patient requires long-term follow-up (Fig. 4).
Discussion
RDD was first described in 1965 by Destombes and later rede-fined in 1969 by Rosai and Dorfman [1–3]. As the disease is extremely rare, there is a paucity of contemporary articles, and its pathogenesis is not yet fully understood. Some recent articles have suggested its association with IgG4-related diseases, but this is still being debated [4,5].
RDD, also known as sinus histiocytosis with massive lymphadenopathy, is characterized by lymph node invasion in 33% of patients [2]. While it can invade lymph nodes all over the body, it primarily invades those in the head and neck region. Central nervous system (CNS) invasion is usually limited to dura-based, extra-axial areas, and rarely involves the cerebrum or spinal cord. Patients with CNS invasion present with location-based neurological symptoms, such as headache, seizure, muscle weakness, and paresthesia [6]. Extranodal invasion occurs in more than 40% of patients and can occur in the skin, nasal cavity, bone, CNS, and gastrointestinal tract. The head and neck are the most vulnerable areas for skin invasion, fol-lowed by the torso [1,3].
RDD reportedly displays “massive” (i.e., ≥7 cm) cervical lymphadenopathy. However, a recent report of 64 patients with RDD from 1994 to 2017 reported that their lymph node size was much smaller, ranging from 1 to 2 cm [2]. This is sim-ilar to the findings in our case, where the patient had incon-spicuous lymph node enlargement.
RDD should be distinguished from other lymph node-involving diseases, including Langerhans cell histiocytosis, reactive lymphoid hyperplasia with sinus histiocytes, and malignant lymphoma [7]. RDD closely resembles other histiocytic disor-ders; however, the rare incidence of hepatomegaly is noticeably different [3]. A biopsy is required for an exact diagnosis.
Emperipolesis, in which histiocytes engulf intact lympho-cytes into their clear cytoplasm, is a characteristic finding, but its presence is not sufficient to diagnose RDD [8]. An immu-nohistochemical study is required to exclude other histiocytic disorders. In RDD, histiocytes are CD1a negative, S-100 positive, and CD68 positive, while Langerhans cell histiocytosis is CD1a positive [1].
The morphology and histology of cutaneous RDD skin lesions show the same features as classical RDD. Therefore, biopsy results cannot distinguish between classical and cutaneous RDD [9]; cutaneous RDD can be re-diagnosed as classical RDD if other symptoms are observed.
Elevated erythrocyte sedimentation rate levels and hyper-gammaglobulinemia with reversal of the albumin: globulin ratio can be seen in classical RDD. Screening tests for Epstein-Barr virus, cytomegalovirus, human herpes virus-6, human herpes virus-8, and human immunodeficiency virus can help to exclude other possible diseases [3,9].
Imaging studies are usually not necessary for diagnosis but can be useful for follow-up and evaluation of treatment re-sponse. Imaging plays an important role in the detection of CNS involvement. On CT scans, RDD CNS involvement ap-pears as a hyperdense lesion, and on MRI as a T1 isointense, T2 isointense, diffusion isointense lesion in the gray matter. Positron emission tomography-CT can also detect CNS involvement and shows increased fluorodeoxyglucose uptake in the lymph nodes [10,11].
Approximately 50% of patients with RDD experience spontaneous remission without any specific treatment. Treatment is only needed when vital organs are involved, or when patients have isolated lesions that can be removed [1,6]. For ex-ample, excision is the preferred treatment option for isolated skin lesions. Approximately one-third of the patients who have undergone surgery experience relapse. Steroid therapy is widely used for recurrent RDD, but guidelines for standard dosage and duration have not yet been established [3].
In our case, the patient showed no more recurrence on the operation site even though she did not receive steroid therapy. Therefore, we suggest that steroid therapy for recurrence of cutaneous symptoms in RDD patients may not be essential. Other symptoms besides the skin lesion may still occur; follow-up every 6 months for the first 2 years and an annual fol-low-up afterwards are needed. Whenever other symptoms ap-pear, patients should immediately undergo investigation [3,9].
This case report describes the process of diagnosing classical RDD from a chronic skin wound which was the only apparent symptom and highlights the importance of considering RDD in patients with skin lesions involving ulcers, especially when accompanied with lymphadenopathy, even though it is a rare disease. In addition, we support the idea that excision and biopsy of skin lesions are viable options for exact diagnosis of RDD and ensuring cosmetic satisfaction.
















