Introduction
Dorsal dislocation of the metacarpophalangeal (MCP) joint is usually caused by a sudden force eliciting hyperextension of the joint. Such dislocations are most often seen in the “border” fingers, the index and little fingers. Without complicated intervening structures, dislocation may be anatomically reduced by simple manual maneuvers, flexing the wrist and applying distal traction with gentle force in the volar vector of the phalangeal base. Uncommonly, soft tissue structures interpose between the metacarpal and the proximal phalanx and result in a fixed “complex” dislocation that is irreducible by closed reduction [1]. Kaplan [2] described this injury in detail in 1957, suggesting that puckering of the volar skin overlying the injured joint combined with X-rays showing dorsal dislocation in the lateral view and widened joint space in the anteroposterior view indicated this diagnosis.
As the single most important obstacle that prevents reduction is the volar plate that is displaced between the metacarpal head and the proximal phalangeal base, surgical reduction requires returning this structure to its original location. However simple this may seem, the dislocation results in heightened tension of the periarticular structures which act as a noose, “locking” the bones and squeezing the volar plate in between. Efficient access to the volar plate while preserving the surrounding neurovascular bundles is the common goal of all surgical approaches.
This is a description of such a case accompanied by a review of the pathological anatomy and treatment armamentarium. This case study was approved by the Institutional Review Board (IRB) of the Catholic Medical Center (IRB No. UC21ZASI0077). The patient provided written informed consent for the publication and the use of his images.
Case
A 16-year-old male sustained a hyperextension injury of his right index finger while being kicked by another player during taekwondo. Palmar skin puckering was observed at the level of the distal palmar crease along the right index ray due to dislocation of the MCP joint. If left unattended, there was a possibility of skin ulceration. Flexion of the index finger was limited. No neurovascular abnormalities were detected (Fig. 1). X-rays revealed dorsal dislocation of the index proximal phalanx and an avulsion fracture of the ulnar aspect of the second metacarpal head (Fig. 2). Manual reduction had been attempted at another hospital but had failed. Computed tomography depicted the displaced volar plate and flexor tendons (Fig. 3).
Fig. 1.
Physical examination on presentation. (A) Palmar view. Puckering of the skin is seen at the level of the metacarpophalangeal joint (distal palmar crease) of the right index finger. (B) Dorsal view.

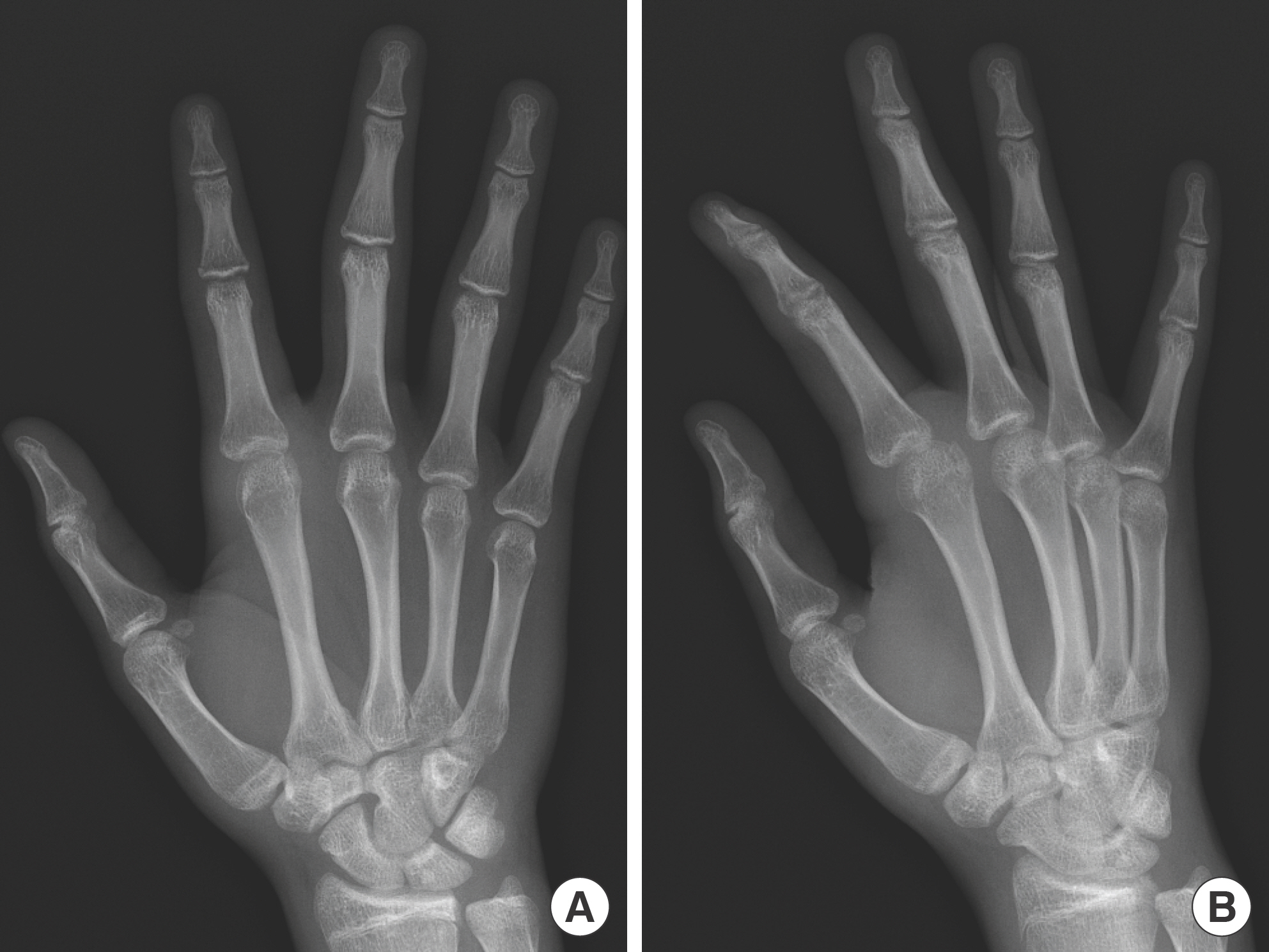
Fig. 2.
Preoperative X-rays. (A) Anteroposterior view shows an avulsed bone fragment of the second metacarpal with widening of the metacarpophalangeal joint space. (B) Oblique view reveals the dorsal dislocation of the proximal phalanx.

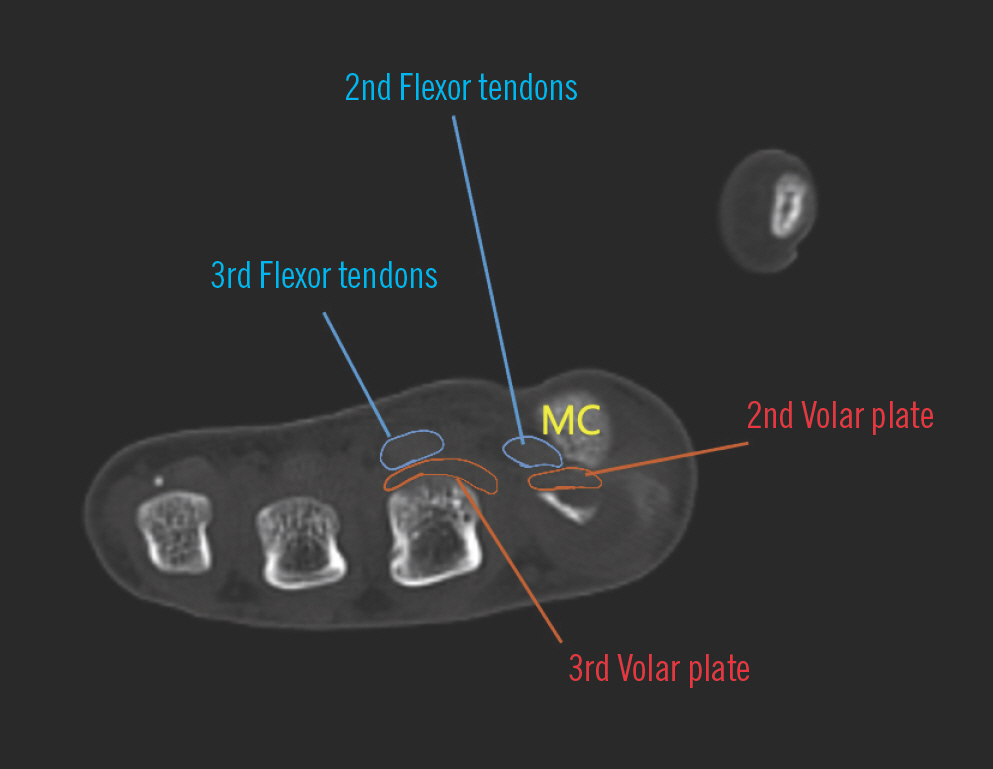
Fig. 3.
Computed tomography of the metacarpal (MC) heads. The flexor tendons have been displaced ulnar to the second MC, and the volar plate is seen dorsal to the MC head. The positions of the intact structures of the middle finger have also been high-lighted for comparison.
Under general anesthesia, a volar Brunner's incision was performed under loupe vision to avoid neurovascular injury. The metacarpal head was protruding beneath a thin layer of soft tissue, and the neurovascular bundles were at the ulnar and radial sides of the bone. The flexors were impinged ulnar and dorsal to the metacarpal, while the volar plate had been completely ruptured from its proximal attachment on the metacarpal (Fig. 4). The flat surface of a Freer elevator was slipped between the volar plate and the proximal phalanx, then pulled palmarly to expose and bring the proximal edge of the volar plate into the visible surgical field. This maneuver was performed along the ulnar side of the metacarpal head, simultaneously releasing the flexor tendons. Beginning at the proximal edge, and taking care that no other structures were damaged, the volar plate was incised in a longitudinal direction. This volar incision functioned as an opening that enabled the metacarpal head to return to its anatomical location dorsal to the volar plate (Fig. 5). With the release of the volar plate, tension around the metacarpal head relaxed, allowing manual reduction of the joint. The loose slips of the volar plate were wrapped around the head of the metacarpal and closed with absorbable sutures (Fig. 6). An additional dorsal ulnar incision was made to aid reduction of the avulsed bone fragment. Bone fragment reduction was achieved by soft tissue realignment, and no additional fixation was necessary. After skin closure, a dorsal block splint was applied. Active flexion exercises were encouraged immediately after recovery, and extension exercises were initiated at 2 weeks after surgery. The splint was removed at 3 weeks. Bony union of the fractured metacarpal head was observed on radiographs 1 month after surgery (Fig. 7). The patient recovered complete range of motion by 6 months after the operation.
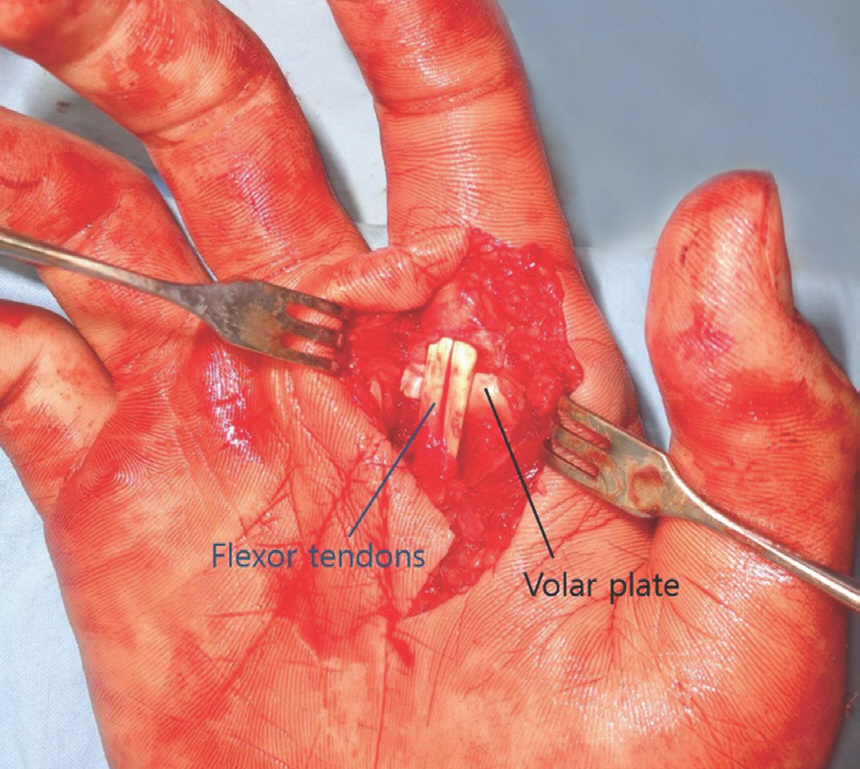
Fig. 4.
Volar approach to the metacarpal head. The radial neurovascular bundle is further displaced to the radial side and the flexor tendons displaced to the ulnar side.
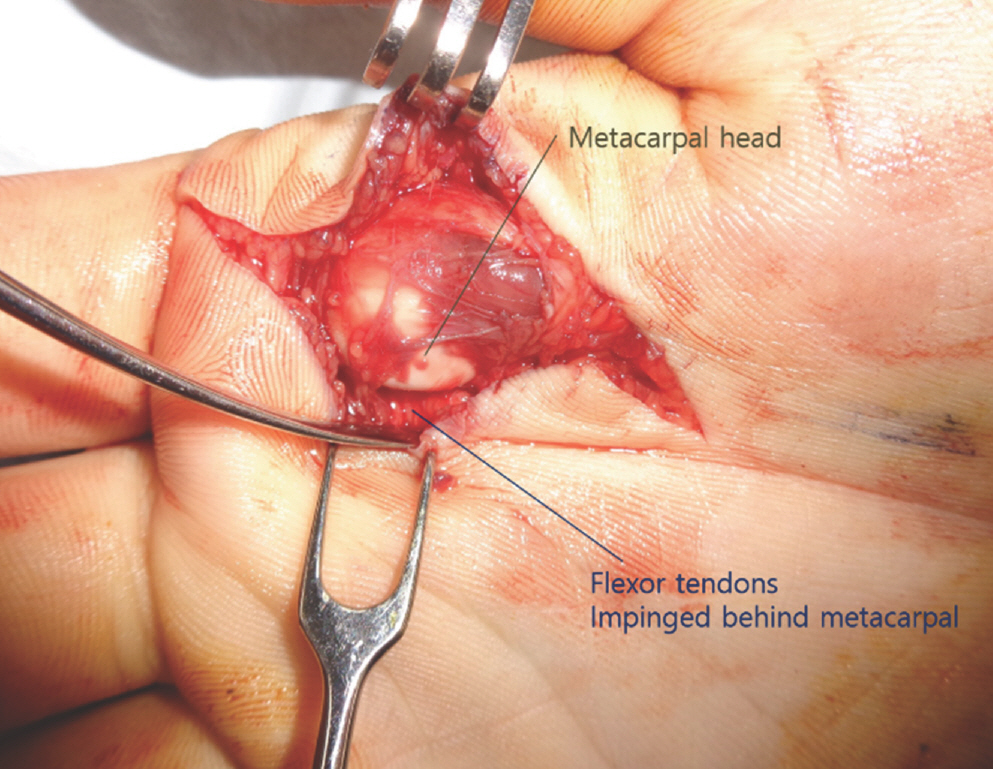
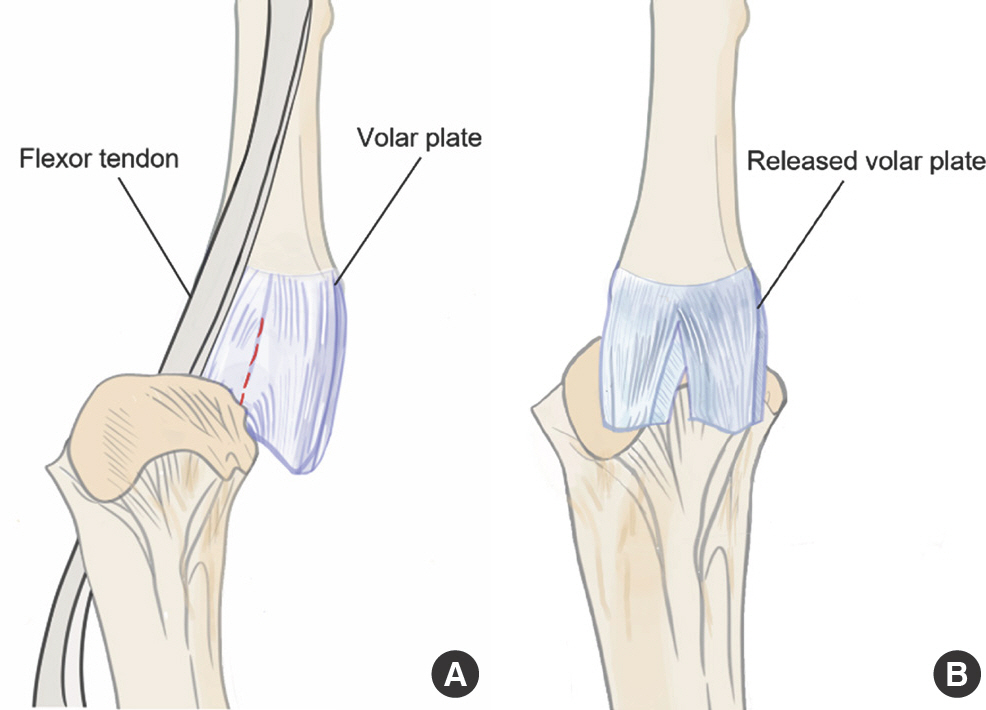
Fig. 5.
Schematic diagram showing ruptured volar plate with dislocation. (A) The ruptured volar plate is displaced dorsal to the metacarpal head. The red dotted line marks the longitudinal volar plate incision line. (B) The released slips of the volar plate were wrapped around the head of the metacarpal after reduction.
Discussion
Complex dorsal dislocation of the MCP joint usually occurs as a complication of a forceful hyperextension injury. The head of the metacarpal bulges out toward the palm, and the base of the proximal phalanx slips dorsal to the metacarpal, pulling the periarticular structures dorsally. The normal periarticular structures of the MCP joint include the volar fibrocartilaginous plate, proper and accessory collateral ligaments, dorsal joint capsule, deep transverse metacarpal ligament (DTML), superficial transverse metacarpal ligament (STML), natatory ligament, sagittal bands, flexor tendon apparatus, lumbricals, interossei, and neurovascular bundles.
Kaplan [2] was the first to vividly describe the pathogenesis of irreducibility, suggesting that a noose formed by the natatory ligament, the STML, the flexor tendons and the lumbricals prevented reduction. The pathological anatomy is relevant to treatment because the culprit that causes the joint to “lock” will be the main target of release. Alternative theories proposed that the DTML, adjacent to the volar plate, forms a band with the plate dorsal to the metacarpal head, and therefore releasing either the volar plate or this ligament would facilitate reduction [3]. In 2009 Afifi et al. [4] developed a cadaveric model of MCP joint dorsal dislocation using a servohydraulic testing machine that delivered a controlled amount of impact load to the index MCP joint of stabilized cadaver hands. In the six specimens that developed irreducible MCP joint dorsal dislocations, they found that the flexor tendons were ulnarly displaced with the A2 pulley intact, and the lumbrical muscle was displaced radial to the metacarpal head. The radial digital nerve was superficial or radial to the metacarpal head. The natatory ligament was distal to the dislocation, and the STML was superficial to the neck of the metacarpal. Performing staged, controlled division of the structures, the authors noted that release of the natatory ligament, STML, flexor tendons and lumbricals did not allow reduction. They described that releasing the DTML, with its continuity to the volar plate, allowed mobility of the volar plate, but the single most important process was release of the volar plate [4].
Although the majority of reports focus on the volar plate, the primary structure responsible for irreducibility may vary for each case. Orozco and Rayan [5] experienced a patient in which the primary structure involved was the first dorsal interosseous muscle and tendon, and the secondary structure was the transverse ligament of the palmar aponeurosis.
Both the dorsal and volar approaches have been advocated for surgical treatment. The volar approach, described by Kaplan [2], heads directly toward the metacarpal head to visualize the pathology and simultaneously access the volar plate. As the displaced volar plate is not directly seen via this surgical window, the greater advantage this method has is for subsequent repair of the divided plate [6]. While Chadha and Dhal [7] warned of injury to the neurovascular bundle that was at times vulnerably tented over the metacarpal head almost directly beneath the level of skin incision, others argue that direct visualization makes protection easier.
With the volar approach, some surgeons have reported that a second dorsal incision was necessary for successful reduction [8]. The volar plate is no longer in a volar location, but sandwiched between the proximal phalanx and metacarpal, therefore equally difficult to access from either approach. Thus more recent studies have advocated for the dorsal incision, as described by Farabeuf [9], which allows excellent exposure of the volar plate, and also has a lower risk of directly transecting the neurovascular anatomy. Vadala and Ward [6], in their comparative retrospective analysis, found that the dorsal approach alone decreased operative time, and did not require a second incision for reduction. The one handicap would be that it is not possible to repair the volar plate, a procedure necessary to prevent repetitive dislocation.
Alternatively, the lateral approach may be an option in cases involving the index or little finger. Pereira et al. [10] suggest that this method provides a view of both the dorsal and volar structures, allows direct reduction of any osteochondral fragments, and avoids risk of tendon adhesion or scar contracture along the axis of motion. However, as with the volar approach, care is required for neurovascular structure preservation.
Minimally invasive procedures have also been reported, mostly in pediatric patients, but not in a large case series. Kodama et al. [11] described using arthroscopy for the MCP joint of the index finger, and were able to achieve volar plate reduction without division. Such methods can be implemented under local anesthesia, sparing the patient the risk of general anesthesia. However, the reproducibility of these procedures has not been reviewed, arthroscopy can require a steep learning curve, and repair of the volar plate is limited.
While there is no consensus on what the single best approach for treatment is, all studies agree that making a correct diagnosis is of utmost importance. Dorsal dislocation seen in imaging studies accompanied by puckering of palmar skin at the level of the dorsal palmar crease is pathognomic. Sesamoid bone trapped in the joint space is also an indicator [12]. Computed tomography or magnetic resonance imaging may reveal the displaced volar plate and flexor tendons but diagnosis is usually based on physical findings and plain X-rays [13].
Um et al. [14] previously reported a case of an open Kaplan's lesion of the little finger managed with open reduction via a volar approach. The pathophysiology of the lesion is analogous to our case; however our case was a closed lesion and therefore more difficult to diagnose upon presentation. Closed complex dorsal dislocations also carry a risk of neurovascular bundle injury during volar incision and approach.
While the authors in Um's case were able to reduce the volar plate without additional incisions, the rupture in this case was limited to the proximal margin, and therefore reduction was impossible without a vertical opening. Our patient also differed in that the lesion occurred on the index finger and was accompanied by an avulsion fracture of the metacarpal.
Early rehabilitation is essential to prevent joint contracture and recover complete range of motion. Rubin et al. [15] mention that even 10 days of immobilization may result in joint stiffness. If the joint regains stability after reduction, there is no reason not to begin controlled range of motion exercises beginning on the day after surgery. To protect the freshly repaired volar plate, the patient should be informed to take care not to hyperextend the joint. A dorsal protective splint should be applied to prevent passive hyperextension but removed during exercise. Full comprehensive flexion and extension should be maintained throughout the scar remodeling period. Any lateral instability may benefit from buddy taping to the adjacent finger during exercise [2].
Without the correct diagnosis, treatment, and rehabilitation, complex dorsal dislocation of the MCP joint will cause severe limitation of motion and joint instability, and may result in arthritis or even aseptic necrosis [15]. This injury is not common, but timely open reduction and rehabilitation can enable full recovery. Therefore the physician should be aware of the possibility of this diagnosis when encountering such a patient.