Introduction
Pressure ulcers are a common problem in older patients, patients with spinal cord injuries, and those with acute illness, and can lead to a variety of complications. Pressure ulcers require repeated treatment over a long period and thus pose a significant burden to the patient as well as society [1,2]. During surgical treatment of pressure ulcers, the ulcer and the ischemic tissue, underlying bony prominence, and bursa must be removed, and in many cases the resulting skin defect must be reconstructed using a flap [2]. Even after a successful reconstruction, complications such as wound dehiscence, seroma, infection, and ulcer recurrence are common [3]. Among these complications, seromas—which refer to the accumulation of serous fluid in the dead space within the flap—may delay wound recovery or lead to infection, wound dehiscence, and skin flap necrosis [4]. Seromas are reported to occur in approximately 25% of patients undergoing pressure ulcer reconstruction, underscoring the critical need to establish more effective strategies for treating and preventing seromas [5].
Seromas are currently treated using various modalities, including surgical revisions (e.g., capsulectomy), aspiration, suction drainage, compression therapy, triamcinolone injections, and sclerotherapy [6]. However, there is no gold standard for seroma treatment, and the specific method of treatment is chosen by the clinician. Viscum album extract is a drug used to treat malignant pleural effusion during pleurodesis. Its safety and efficacy as a sclerosing agent have been confirmed by several studies [7,8]. Furthermore, several reports have described the successful treatment of seromas in the flap donor site using V. album extract [9].
Here, we report three cases in which surgery and sclerotherapy using V. album extract were effective in treating seromas that had developed following pressure ulcer reconstruction.
Case
We conducted a retrospective review of patients who underwent pressure ulcer reconstruction followed by additional sclerotherapy using V. album extract (Abnobaviscum F; Abnoba Heilmittel GmbH, Pforzheim, Germany) to treat and prevent seromas. All patients were treated at a single hospital and provided informed consent for the publication of their clinical and radiological data. The study was approved by the Institutional Review Board of Chonnam National University Hospital (CNUH-EXP-2021-364). The patients underwent surgery for soft tissue defects caused by pressure ulcers or seromas that had occurred after a previous reconstruction. Wide debridement including capsulectomy was performed, followed by reconstruction using a local flap. Progressive tension sutures were used in all patients to minimize dead space. A Hemovac drain was placed on the wound bed upon closure for suction drainage. To prevent the V. album extract solution from leaking between the wound margins and affecting the surrounding skin during the procedure of sclerotherapy, we additionally use topical skin adhesives on the sutured margins. Simple dressing with antibiotic ointment and Vaseline gauze was performed until postoperative day (POD) 4, and compressive dressing with fluffy gauze was performed beginning on POD 5. Patients remained in the prone or lateral decubitus position for at least 4 weeks after surgery.
All three patients received sufficient explanation regarding the application of sclerotherapy to prevent the development or recurrence of seromas and consented to treatment. Fluid that had accumulated inside the wound was completely removed through a Hemovac line, and the drained volume was measured. Afterwards, a fluid mixture of V. album extract and normal saline was injected through the Hemovac line, and the line was clamped. In the first procedure, 2 mg of V. album extract was mixed with 10 mL of normal saline. If the seroma had not resolved even after 2 weeks, a second procedure was performed with a fluid mixture of 4 mg of V. album extract and 10 mL of normal saline (Table 1). After injecting the fluid, the patients were instructed to change their positions between prone, right lateral, and left lateral at 10-minute intervals. As much of the injected fluid as possible was removed through the Hemovac line 30 minutes after the first injection. The Hemovac was emptied once a day to check the volume, color, and odor of the drained fluid, and the Hemovac was removed when less than 10 mL of fluid was drained for 2–3 consecutive days and no fluctuations or inflammation was observed around the wound during physical examination.
Case 1
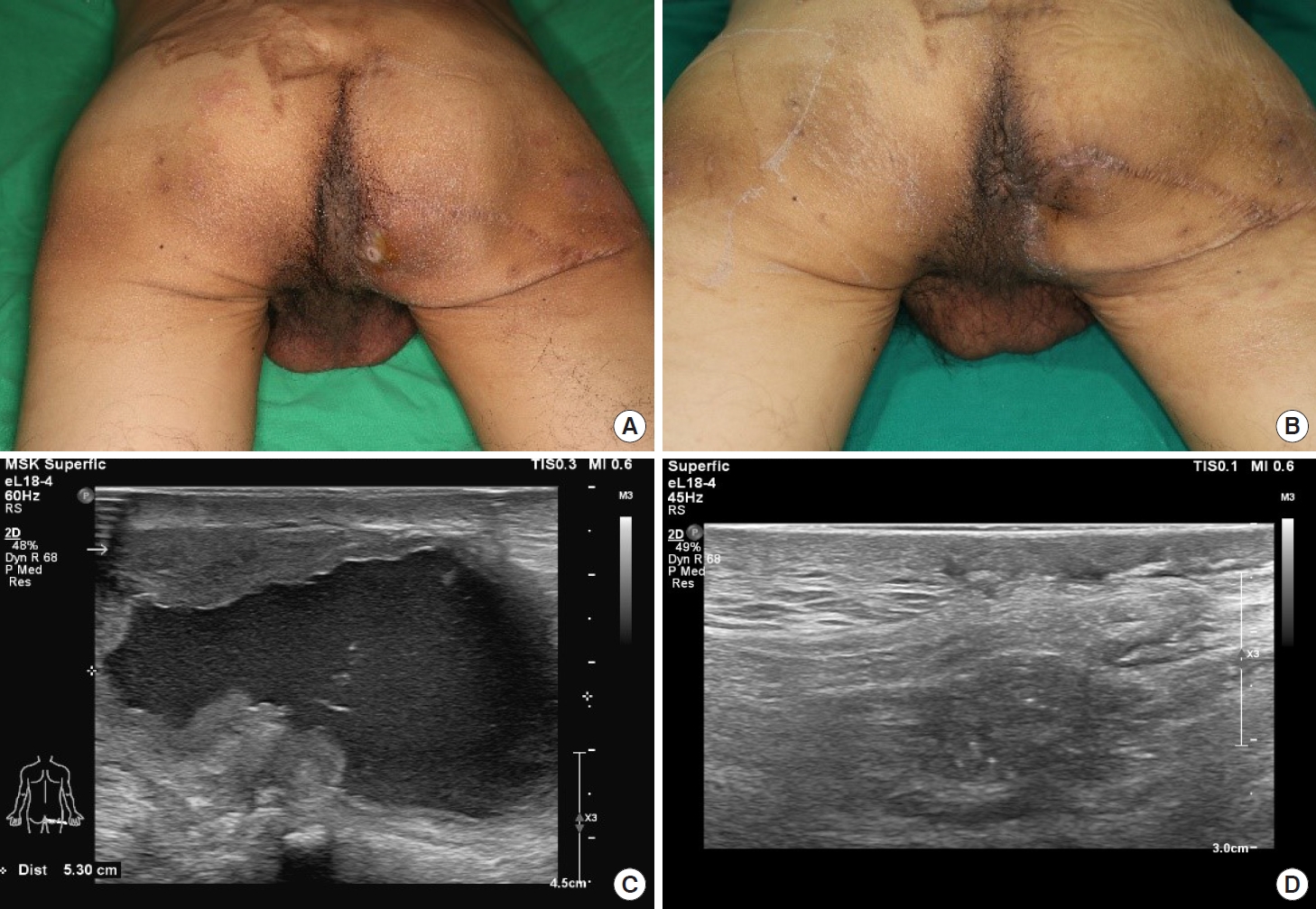
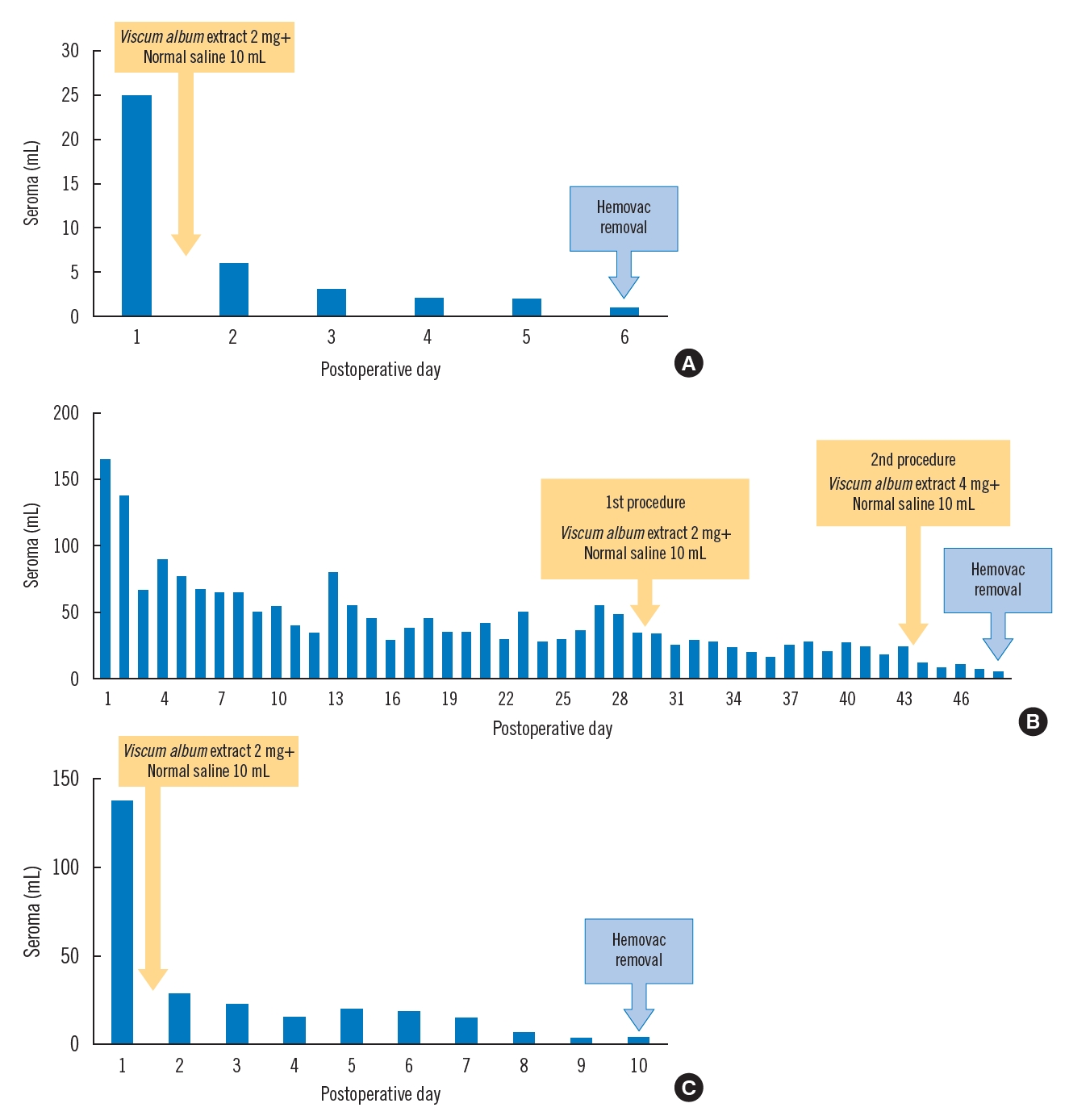
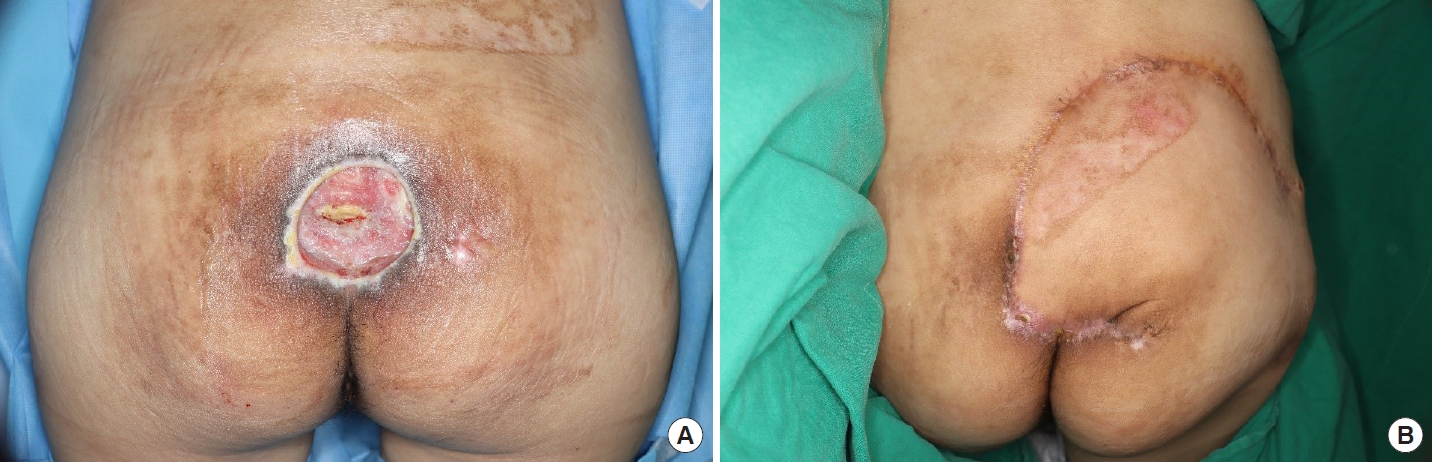
A 49-year-old male patient with paraplegia due to a previous motorcycle accident exhibited palpable fluctuations and mild wound dehiscence around the right ischial area (Fig. 1). He had undergone debridement and local flap reconstruction for a pressure ulcer in the right ischial area in our plastic surgery department 6 years earlier. Since then, the patient had experienced recurrent seromas, for which two revision procedures were performed (1 year and 8 months earlier, respectively). Preoperative ultrasonography (US) revealed a 4.3×5.3-cm area of fluid collection (Fig. 1). Hence, capsulectomy and local advancement flap procedures were performed. The first sclerotherapy procedure was performed on the day after surgery. There was a clear reduction in the volume of drained fluid, and the Hemovac was removed on POD 6 (Fig. 2A). The patient recovered fully and was discharged without developing wound dehiscence or other complications, and no signs of seroma have been observed on US as of 1 year after surgery.
Case 2
A 49-year-old male patient with quadriplegia due to a cervical spine injury related to a previous traffic accident developed a pressure ulcer in the coccygeal area, which was observed as a 6×5-cm soft tissue defect partially exposing the coccyx and sacrum (Fig. 3). Thus, wide debridement and reconstruction using a right gluteus maximus musculocutaneous rotation flap were performed. Before the surgery, we provided an explanation of sclerotherapy using V. album extract, but the patient refused; hence, only conservative treatment was performed. However, the volume of drained fluid had not resolved 1 month after surgery, and pelvic computed tomography images taken 1 month after surgery showed fluid collection in the wound without capsulation. Thus, we consulted the patient, who then elected to undergo sclerotherapy using V. album extract. After the first sclerotherapy procedure, the volume of drained fluid had decreased slightly, although the seroma had not resolved. A second sclerotherapy procedure was therefore performed (Table 1). Thereafter, the volume of fluid decreased, and US performed 6 months after discharge indicated no signs of seroma (Fig. 2B).
Case 3
A 57-year-old male patient with paraplegia due to a thoracic spine injury incurred during a fall developed a pressure ulcer in the sacral area, which was observed as an 8×8-cm soft tissue defect exposing the sacrum (Fig. 4). Wide debridement and reconstruction using a right gluteus maximus musculocutaneous rotation flap were performed. The first sclerotherapy procedure was performed on the day after surgery. Although the medical staff observed a mild increase in heat within a localized area around the surgical site on the day after sclerotherapy, it had improved by the next day. There was a clear reduction in the volume of drained fluid, and the Hemovac was removed on POD 10 (Fig. 2C). The patient fully recovered and was discharged without wound dehiscence or other complications, and no signs of seroma or other complications have been observed as of 6 months postoperatively.
Discussion
Seromas are common complications of various surgeries, including flap surgery. The flaps must be well secured, and primary union must be achieved with minimal granulation tissue for the soft tissue defect or surgical site to heal properly. However, in pressure ulcer reconstruction, there is a high risk of dead space creation beneath the flap during surgeries that involve soft tissue defects or extensive dissection, and shear force hinders flap fixation, thereby hampering the formation of a collagen matrix for wound recovery [3,4]. In patients with pressure ulcers, the surrounding tissues, including the skin, are more easily damaged by external factors, and patients are exposed to a shearing force for more prolonged periods due to their limited mobility, thus leading to reduced blood and lymphatic flow in the affected area. For these reasons, dead spaces form more easily beneath normal skin or reconstruction sites, fluid collection occurs, and persistent or recurrent seromas often develop [6,10].
Seromas are asymptomatic and spontaneously absorbed in most cases, but they sometimes cause discomfort or lead to inflammation, wound dehiscence, and flap necrosis, which then necessitate additional surgical treatment. Furthermore, the normal wound healing process may be delayed, as seromas hinder the contact between the flap and surrounding tissue [4]. Such symptomatic and non-absorbed seromas can be treated by removing internal fluid through repeated aspiration and suction drainage or by using corticosteroid injections, providing compression using a garment or dressing, or sclerotherapy. Seromas that do not respond to conservative treatment or have developed fibrous pseudocapsules must be surgically removed via capsulectomy, and the resulting defect must be reconstructed via flap surgery. Previous studies have indicated that minimizing dead space during these procedures by using a tissue adhesive or performing sclerotherapy can help lower the risk of seroma [4,11].
Numerous drugs such as talc, iodopovidone, doxycycline, minocycline, bleomycin, autologous blood, and OK432 have been used to treat seromas or malignant pleural effusion. Although the most effective drug remains to be identified, V. album extract is a newly introduced chemical agent that has been extensively studied given its low risk of adverse reactions and good therapeutic effects [8]. One of the ingredients of V. album extract is viscumin, which is intensely toxic. Viscumin inhibits the binding of leucine in cell faster than that of uridine and thymidine. The toxin inhibits cellular protein synthesis [12]. V. album extract exerts antitumor effects by preventing protein synthesis and inducing cell death. Furthermore, it aids in eliminating dead space through immune responses that stimulate the synthesis of macrophage colony-stimulating factors and increase the concentrations of interferon, interleukins, tumor necrosis factors, and natural killer cells [9]. Treatments using V. album extract have been reported to lead to mild adverse events such as local heat sensations and local pain, which tend to resolve shortly afterward [7,8]. In fact, one of our patients experienced a local heat following V. album extract injection, which had improved by the next day without systemic fever or other complications. Although major complications from using V. album extract are known to be rare, it is not advisable to use on pregnant patients unless absolutely necessary.
To date, there have been no reported cases of sclerotherapy using V. album extract following surgical reconstruction for a pressure ulcer. In the present cases, we performed surgical treatment and sclerotherapy using V. album extract in a patient with a recurrent seroma, a patient with a persistent seroma, and a patient wishing to undergo sclerotherapy immediately postoperatively as a prophylactic treatment. None of the three patients developed serious complications, and all patients experienced quick recovery after treatment without recurrence of seroma. These cases suggest that sclerotherapy using V. album extract is safe and effective for preventing and treating seromas that develop following pressure ulcer reconstruction or surgical seroma treatment, allowing for reductions in dead space with few complications. Nonetheless, further studies with larger sample sizes, more varied demographics, and longer follow-up periods are required to verify these findings.