Introduction
The parotid gland or duct can be injured due to deep lacerations of the cheek or surgical procedures such as parotidectomy, rhytidectomy, mastoidectomy, and skin tumor resection. These injuries cause abnormal leakage of saliva into the wound, and autolytic enzymes in salivary secretions can critically impair wound healing. Therefore, these injuries should be detected early and repaired properly to return parotid function to normal [1]. However, early diagnosis and appropriate management are often delayed or missed, which may result in serious complications such as sialocele or parotid fistula. Even if such injuries are found early and repaired adequately, salivary leakage can develop as a complication. Salivary leakage is very distressing, both to the patient and to the surgeon, because conservative and surgical treatments are often unsatisfactory. In order to heal wounds complicated by the leakage of saliva caused by parotid injury, it is necessary to reduce or stop salivary secretions for an adequate period. Before the introduction of botulinum toxin for clinical use, various treatment modalities had been used for this purpose, including restriction of oral intake, anticholinergic drugs, tympanic neurectomy, radiation, and parotidectomy, with varying results [2-7]. Meanwhile, over the last two decades, researchers have advocated injecting botulinum toxin type A into the parotid gland as an alternative treatment option to decrease salivary secretions, and multiple reports have confirmed that botulinum toxin A is effective for treating parotid fistula or sialocele [8-14]. Herein, we present five cases involving parotid gland or duct injuries that were successfully treated with botulinum toxin A injection (Table 1).
Methods
A retrospective study was conducted to evaluate the efficacy of botulinum toxin A for treating salivary leakage from parotid gland or duct injuries. Five patients were treated between 2011 and 2016, three of whom received postoperative injections with a total dose of 30–40 units of botulinum toxin A (Botox, Allergan, Irvine, CA, USA) after reconstituting a 100-unit vial with 3 mL of normal saline. One of the other two patients was injected with the same amount of botulinum toxin A preoperatively, and the other received an intraoperative injection. The toxin was injected into four to eight sites of the parotid gland with a divided dose using an insulin syringe or a 1 mL syringe with a 30-gauge needle, and in one patient, the injections were made under ultrasonographic guidance. In the other four patients, the toxin was injected without the aid of imaging tools. This study was approved by the Institutional Review Board (IRB) of Kangwon National University Hospital (IRB No. KNUH-2020-12-003). The patients provided written informed consent for the publication and the use of their images.
Results
All five patients showed an abrupt decrease of salivary leakage on the 3rd day after the toxin injection and exhibited satisfactory wound healing without untoward side effects. No recurrence was observed in any of the five patients during follow-up periods ranging from 3 to 20 months.
Case presentations
Case 1
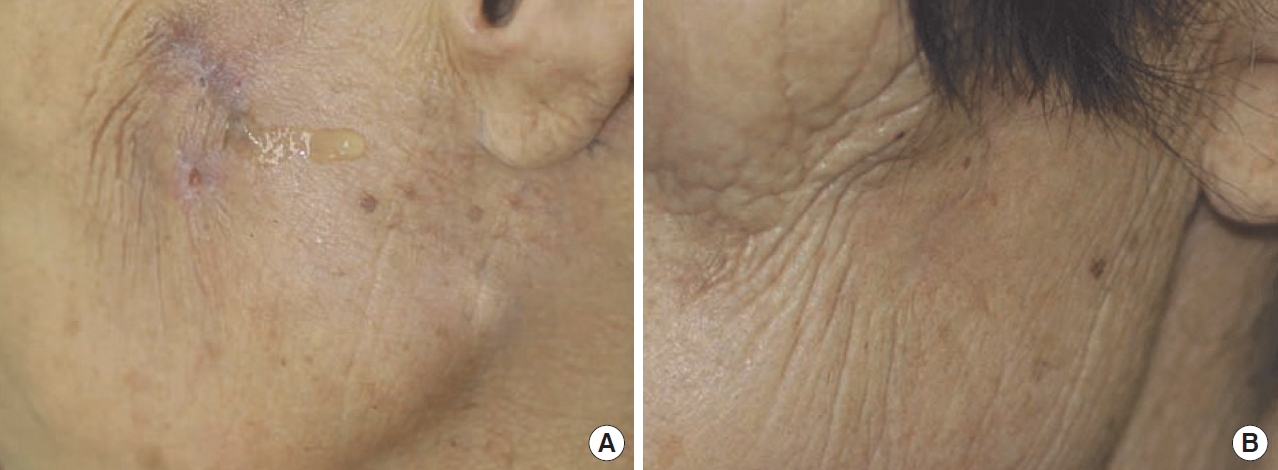
A 72-year-old woman presented with watery, clear discharge from a very small opening on her left cheek. The discharge had lasted for 6 months and increased during food intake. Her medical history revealed acute suppurative parotitis 6 months earlier. At that time, she was treated with incision and drainage, followed by antimicrobial medication. On physical examination, there was a 2 mm-diameter opening with surrounding scar tissue on the left cheek (Fig. 1A). Laboratory analysis of the fluid revealed an elevated amylase level (more than 300,000 IU/mL), which confirmed saliva leakage from a parotid fistula. The left parotid gland was demarcated by a radiologist with an ultrasound scan, and 40 units of Botox were injected preoperatively into four separate subdivisions of the left parotid gland in divided doses. On day 3 after the injection, the discharge from the left cheek began to decrease and ceased completely on day 5. On day 7 after botulinum toxin injection, fistulectomy was performed under local anesthesia. The wound healed well without any complication. The postoperative course was uneventful at the 13-month follow-up (Fig. 1B).
Case 2
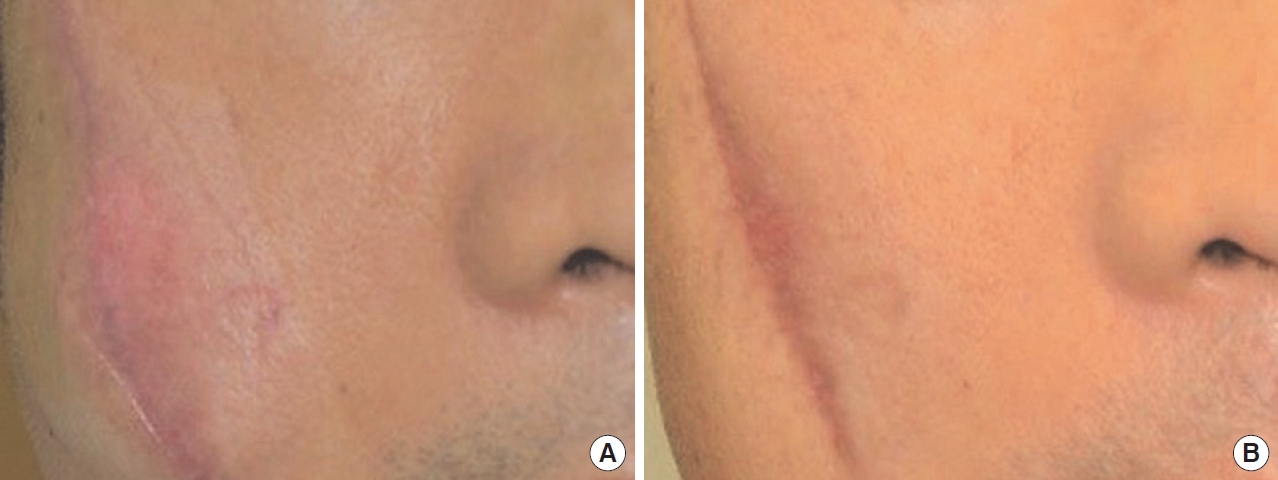
A 47-year-old man was injured on his left cheek by glass. On his visit to emergency room, only skin laceration was repaired after insertion of a silastic drain (Fig. 2A). In response to gustatory stimuli after skin repair, profuse clear fluid discharged out of the drain site. Under the impression of a parotid duct injury, his cheek was explored on the next day and the severed parotid duct was repaired after inserting a silastic stent. However, leakage of saliva developed on the next day, and did not stop despite conservative management including restriction of oral food intake and compression. On postoperative day 7, 40 units of Botox were injected into five sites in the left parotid gland in divided doses. The leakage stopped 5 days after the botulinum toxin A injection. The silastic stent was kept for 3 weeks. The patient has remained well during 20 months of follow-up (Fig. 2B).
Case 3
A 48-year-old man was injured deeply on his right cheek by a sharp metal object. An emergency operation was performed to explore and repair the wound. Injuries of the parotid gland parenchyma and the facial nerve (buccal and zygomatic branch) were repaired with caution. Oral food intake was not allowed for 5 days after the operation. On starting oral intake on postoperative day 6, his cheek became swollen (Fig. 3A). Under the impression of salivary leakage into the wound, a total of 40 units of Botox were injected at eight sites of the right parotid gland in divided doses. On day 3 after toxin injection, leakage of saliva began to decrease gradually. The wound healed well eventually. No recurrence was found at the 3-month follow-up (Fig. 3B).
Case 4
A 76-year-old woman underwent surgical excision for a squamous cell carcinoma on her right cheek. During the operation, a small part of the parotid duct was resected because of tumor invasion, during which the parotid capsule was injured inadvertently. After repair of the parotid capsule and ligation of the proximal Stensen duct, 30 units of Botox were injected at six sites on the right parotid gland intraoperatively. The open wound after tumor resection was repaired with a rotational skin flap from the neck. For 3 days after the operation, clear fluid collected in the suction drainage bottle despite food restrictions, and the fluid was revealed to be saliva in an amylase test. On postoperative day 4, there was only minimal fluid collection. The wound healed completely by 2 weeks after surgery. No salivary disorders such as fistula or sialocele were observed at a 6-month follow-up.
Case 5
A 71-year-old woman underwent surgical excision for a Merkel cell tumor on her left cheek. During resection of the tumor, the parotid capsule was injured. After repairing the capsule, the surgical wound was covered with a rotational skin flap from the neck. Until the 2nd day after the operation, clear fluid discharged at the drain site, and the fluid was confirmed to be saliva in an amylase test. On postoperative day 3, 40 units of Botox were injected at eight sites into the right parotid gland in divided doses. On the 3rd day after the toxin injection, the clear discharge began to decrease and stopped on day 5. The surgical wound healed uneventfully. The patient has remained well during 3 months of follow-up.
Discussion
Physicians often encounter surgical wounds complicated by abnormal leakage of saliva, which is caused by parotid or duct injuries. In order to achieve desirable results from wound treatment, salivary secretion must be reduced or ceased because the autolytic enzymes in saliva hinder wound healing and cause infection. In the past, several conservative methods such as compressive dressings, suction drainage, food restriction, and anticholinergic drugs have been tried to reduce salivary secretions and promote healing. However, their effects were often disappointing. Prior to introduction of Botox toxin injections for treatment of parotid fistulas, only 50% of patients with longstanding parotid fistulas found success with conventional treatments [7].
Anticholinergic drugs reduce salivary secretions temporarily, but their use has been limited due to their profile of side effects, including palpitation, tachycardia, photophobia, urine retention, blurred vision, and dryness of mouth. In contrast, botulinum toxin only acts on the injected parotid gland and reduces salivary secretions without systemic side effects. Although some surgeons recommend the concomitant use of botulinum toxin with antisialogogue drugs such as scopolamine [15,16] and atropine [17], this is not necessary because the botulinum toxin injection is sufficiently effective on its own to inhibit salivary secretion. Botulinum toxin injection was first proposed in 1997 by Bushara [18] as an alternative approach to manage secretory disorders of the parotid glands. Bushara reported favorable results of botulinum toxin A injection in treating sialorrhea in patients who had amyotrophic lateral sclerosis or other neurological disorders. It has long been known that botulinum toxin A blocks neuromuscular junction and all autonomic cholinergic fibers, including major secretomotor parasympathetic fibers, to the salivary glands. Although botulinum toxin A injection has been frequently used to treat spasmodic torticollis, hemifacial spasm, blepharospasm, and expressional wrinkles for cosmetic use, it has also been applied to treat parotid fistula, sialocele, recurrent parotitis and salivary secretory disorders such as neurologic sialorrhea and Frey syndrome [8-14,18-20].
Parotid fistulas are more frequently associated with gland injuries than with duct injuries. Parotid duct injuries are often overlooked in trauma cases, or are irreparable in cases of severe injuries even if they are recognized. Missed or irreparable parotid duct injuries may eventually result in parotid fistulas, which can be effectively managed using botulinum toxin A. Our study also included a case of parotid fistula caused by duct injury. In acute parotid fistula, the toxin is usually injected postoperatively. However, a preoperative injection is needed to prevent postoperative salivary secretions in chronic fistula cases. An intraoperative injection can also be performed to prevent parotid fistula when an iatrogenic gland injury occurs during surgery.
Some researchers injected the toxin into the parotid parenchyma under ultrasonographic assistance [11,12], and others did so under electromyographic control [10,19]. Although it is not mandatory, preoperative demarcation the parotid gland with an ultrasound scan is very helpful for injecting the toxin into the parotid parenchyma and avoiding untoward side effects. The toxin was injected in our patients using an insulin syringe or a 1 mL syringe with a 30-gauge needle, depending on the thickness of skin and subcutaneous tissue. The appropriate doses and injection techniques to obtain optimal results remain controversial. Capaccio et al. [11] suggested that each parotid gland should receive 25–60 units of botulinum neurotoxin type A (Botox, Allergan), and proposed that the treatment should be fractionated into four doses (for the lower, upper, posterior, and anterior quadrants), none of which should contain more than 15 units. Arnaud et al. [20] used 100 units of Botox, and von Lindern et al. [9] used 450 units of Dysport (Ipsen Pharma) for parotid fistula treatment, corresponding in clinical efficacy to about 150 units of Botox. Jung et al. [15] injected a total of 50 units of botulinum toxin type A (Botulax; Hugel, Inc.) in all injection sites, which were 1 cm apart, with successful results in treating parotid fistula complicated by face lift surgery. In our studies, a total dose of 30–40 units of Botox was used to stop salivary secretion through injections at four to eight sites in divided doses. We injected relatively low doses of toxin compared to the doses used by other researchers, which may inform future research investigating the minimum effective dose to stop salivary secretions. In our study, 30 units of Botox was the minimum dose. However, further investigation should be carried out to determine the adequate dose and proper distances between injection sites to obtain optimal results for managing wounds complicated by salivary leakage. Most of our patients showed an abrupt decrease of salivary secretions on the 3rd day after the toxin injection, and secretions almost stopped around the 5th day.
No postoperative complications were observed in any of the five patients, including the patient with the longest follow-up period of 20 months. Considering that the effect of botulinum toxin A usually lasts from 3 to 6 months, the absence of recurrence in our three patients who were followed up for more than 6 months suggests that repeated toxin injections are not necessary. Instead, a single injection can inhibit salivary secretions for a duration long enough for the wound to heal.
In conclusion, the injection of botulinum toxin type A with a dose equivalent to 30–40 units of Botox is suggested as a safe, effective, and reasonable therapy to manage wounds complicated by parotid gland or duct injuries.