Introduction
Necrotizing fasciitis is an uncommon but life-threatening infectious disease that primarily involves the superficial fascia and subcutaneous tissue [1]. Although it can affect all parts of the body, it most commonly affects the extremities, abdominal wall, and perineum, but it rarely involves the head and neck [1,2]. The predisposing conditions of necrotizing fasciitis are old age (more than 65 years), diabetes mellitus, liver cirrhosis, alcoholism, intravenous drug usage, hypertension, chronic renal failure, malignancy, and immunocompromised state [1-3]. Because this infectious disease progresses rapidly, its mortality rate is noticeably high [1]. Especially in patients with cervicofacial necrotizing fasciitis, notwithstanding aggressive management, the mortality rate is 25.5% [2]. Promptness of diagnosis, aggressive debridement, intravenous antibiotic treatment, and management of complications are required to improve the survival rate [1].
We report the successful treatment of two elderly women with necrotizing fasciitis of the scalp, which was secondary to an odontogenic infection, with negative pressure wound therapy (NPWT). To our knowledge, these are the first reported cases of necrotizing fasciitis of the scalp originating from odontogenic infections. The study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained from the patients for the use of their images.
Cases
Case 1
A 66-year-old woman diagnosed with diabetes mellitus presented to the emergency department with complaints of fever (temperature, 38.7°C), general weakness, and pain and swelling of the left cheek. She used to be a smoker and engaged in alcohol abuse until she was diagnosed with hepatocellular carcinoma. She had a history of left lower dental pain and left mandibular swelling that were treated for 1 week by staff at a local medical center. Her initial C-reactive protein (CRP) level was 39.19 mg/dL. Facial computed tomography (CT) revealed multifocal intramuscular abscess formation, fluid collection, fascial edema, and soft tissue thickening and emphysema from the perioral region to the scalp.
After immediate incision and drainage of the abscesses, she was admitted to the otolaryngology department with a diagnosis of masticator space abscess and started on intravenous cefotetan and clindamycin. Additionally, staff in the oral and maxillofacial surgery (OMS) department extracted the tooth that seemed to be the source of the infection. Despite 2 weeks of treatment, the patient’s state did not improve, and progression of the inflammatory process was observed by CT (Fig. 1). In suspicion of necrotizing fasciitis, the patient was referred to the plastic and reconstructive surgery department, and extensive incision and drainage of the abscesses was performed (Fig. 2A). Preoperatively, the skin was partially necrotized. Intraoperatively, tissues along the fascial plane were easily separated by blunt dissection, which strongly suggested necrotizing fasciitis, and partial necrosis of the temporalis muscle was observed. Every 5 or 6 days, we debrided the necrotic tissue and applied NPWT with a vacuum-assisted closure device (VAC; Kinetic Concepts Inc., San Antonio, Texas, USA). We placed one end of a cut Jackson-Pratt drainage tube (EZ-VAC; Gems, Seoul, Korea) into the deep portion of the wound, through the vacuum foam, and we connected the other end of the drainage tube to the negative pressure vacuum hose (Fig. 3). This procedure facilitated the drainage of discharge from the deepest level of the wound. After consultation with the division of infectious disease within the department of internal medicine, appropriate antibiotics (vancomycin, tazobactam-piperacillin, and ciprofloxacin) were used in accordance with the cultured bacteria (Streptococcus intermedius, Pseudomonas aeruginosa, multi-resistant Acinetobacter baumannii, methicillin-resistant Staphylococcus epidermidis [MRSE], and Corynebacterium striatum).
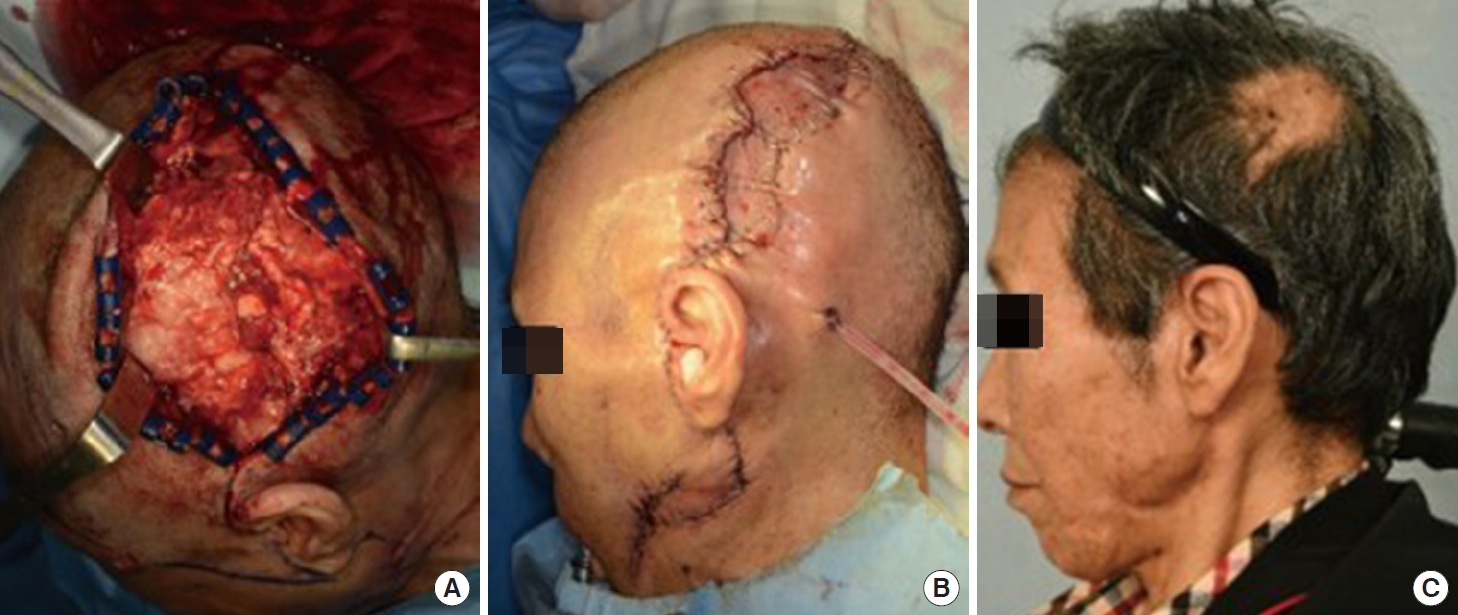
After 24 days from the first day of NPWT, the soft-tissue infection was controlled (CRP, 0.47 mg/dL), and the patient underwent primary closure and split thickness skin grafting with bone decortication. NPWT was also applied to the site of skin grafting (Fig. 2B). The patient’s general condition improved, and she was eventually discharged on hospital day 58. The healed wound at 6 months is shown in Fig. 2C.
Case 2
A 77-year-old woman presented to the emergency department for progressive facial swelling with pain for 3 weeks. Her comorbidities included diabetes mellitus, hypertension, angina pectoris, adrenal insufficiency, and hypercholesterolemia. She also had a tooth extracted at a local dental center 3-month prior. Her initial CRP level was 41.49 mg/dL. A facial CT revealed multifocal fluid collection, soft tissue swelling, and thickening from the perioral region to the scalp.
Aspiration biopsy of the site of multifocal fluid collection was performed immediately, and it showed that the multifocal fluid was an abscess. She was admitted for necrotizing fasciitis, and intravenous antibiotics were injected. Incision and drainage of the abscess were performed by staff in the plastic and reconstructive surgery department and OMS department as soon as was possible. Intraoperative findings were similar to those of the patient in case 1. After 3 days of applying a povidone iodine-soaked gauze dressing, we debrided the necrotic tissue and applied NPWT every 4 or 5 days. We cut the Jackson-Pratt drainage tube and inserted it in the same manner as in the first case. Appropriate antibiotics (teicoplanin, vancomycin, tigecycline, meropenem, and metronidazole) were used in accordance with the cultured bacteria (MRSE, Staphylococcus capitis, C. striatum, Enterococcus faecium, and Candida dubliniensis).
After 26 days from the first day of NPWT, the soft-tissue infection was controlled (CRP, 2.81 mg/dL), and the patient underwent only primary closure. She was discharged on hospital day 53, and she remains in good health at 1 month later. The healed wound at 1 month after wound closure is shown in Fig. 4.
Discussion
Necrotizing fasciitis, a rare but potentially fatal fulminant infection of the superficial fascia and subcutaneous tissue, can result in septic condition, disseminated intravascular coagulation, and/or multiorgan failure that lead to death if inadequately treated [1,2]. Cervicofacial necrotizing fasciitis accounts for about 3% of all cases of necrotizing fasciitis, and only 4% of which involve the scalp [1,2]. Cervical necrotizing fasciitis most commonly originates from a dental infection, unlike craniofacial necrotizing fasciitis, which usually originates from orbital or periorbital disease [4]. Usually, the abscess or infection progresses downward because of gravity. However, in our cases, the fact that the patients were nearly bedridden due to general weakness might have caused the necrotizing fasciitis of the scalp to originate from the odontogenic infection. Especially in the second case, it is unusual for an infection of the mandibular teeth to progress to the scalp. Therefore, to our knowledge, our cases of necrotizing fasciitis of the scalp originating from an odontogenic infection are the first reported cases. Although one of our patients was taking a steroid for adrenal insufficiency and both patients had diabetes mellitus, the desirable clinical outcomes observed in our cases are contributable to the following factors: appropriate and timely surgical/medical treatment, the absence of thoracic extension of necrotizing fasciitis, and the fact that craniofacial necrotizing fasciitis has a mortality rate that is a quarter of the mortality of cervical necrotizing fasciitis [4,5].
NPWT removes fluid and optimizes the wound environment [6,7]. It can manage traumatic, chronic, complex, pressure-related and infected wounds effectively [6-9]. If traditional management, such as a povidone iodine-soaked dressing, had been applied to our patients, the dressing would have had to be changed more frequently because of copious wound exudate. However, use of NPWT enabled effective exudate control, collapse of the wound cavity, and fewer dressing changes, the last of which is generally painful for patients.
A grossly contaminated wound is one of the contraindications of NPWT [10]. However, since NPWT removes excessive edema fluid and decreases the amount of bacteria [8,9], some surgeons have already successfully healed necrotizing fasciitis with NPWT [11-14]. Gillespie et al. [11] treated a 44-year-old man with bilateral periocular necrotizing fasciitis using NPWT and covered the wound with skin graft. Nouraei et al. [13] reported healing the necrotizing fasciitis of the neck using NPWT and skin grafting. Chen et al. [14] reported that NPWT had several advantages compared with conventional debridement and drainage. Necrotizing fasciitis of the head treated with NPWT is relatively rare but has increased in the recent years. Important prerequisites for the use of NPWT are the absence of necrotic tissue and a well-vascularized wound bed. The application of NPWT without adequate debridement of the wound can cause a deeper or systemic infection [15].
When we applied NPWT in these cases, the drainage tube of Jackson-Pratt drain was cut and inserted into the vacuum foam. Because the wound was quite deep but narrow, we applied this method to provide enough negative pressure at the deep portion of the wound to drain the discharge sufficiently. Although the patients initially suffered from severe infection, it was effectively controlled without frequent changes of dressing. This method reduced the patients’ pain and physicians’ effort.
The patients’ general conditions improved, and their surgical wounds healed uneventfully with good outcomes. Since necrotizing fasciitis of the scalp originated from odontogenic infections in both cases, we worked with the OMS department. Wound closure after the administration of appropriate antibiotics, incision drainage, and sufficient debridement with NPWT lead to excellent results and effective degree of recovery.