Introduction
Small free flaps have become an invaluable option for reconstruction of the fingertip. The partial second toe pulp free flap is optimal, providing well vascularized glabrous tissue from the tibial aspect of the second toe. The dimensions of the pedicle are well matched to the digital vessels, and donor site morbidity is negligible [1]. Other options for small volume reconstruction include the great toe pulp free flap, the toe plantar flaps, hypothenar free flap, radial artery superficial palmar branch flap, ulnar artery perforator flap, radial artery perforator flap, dorsoradial artery perforator flap, and dorsoulnar artery perforator flap [2-4].
Insetting the small free flap is relatively straightforward, as most fingertip defects will require anastomosis to one of the digital arteries. Most of the time however, the small cylindrical geometry of the finger is too snug to allow relaxed coverage of the pedicle. Tension on the pedicle may lead to vascular compromise and consequently flap failure. Studies have investigated methods of pedicle coverage, including adipofascial flaps and skin grafts [5,6]. Leaving the pedicle exposed, or coverage with artificial materials may risk desiccation or necrosis [7,8].
Han and Min [9] have studied the safety of applying a split-thickness skin graft (STSG) over the pedicle of a variety of free flaps. They have postulated that the vascular supply from the pedicle directly beneath the graft increases the proportion of graft take. However, the split-thickness graft requires a dermatome for harvest, which is disadvantageous for the tiny areas of skin required on the digit pedicle. An alternative is placing a full-thickness skin graft (FTSG) over the pedicle by obtaining a small area of full-thickness skin, which can come from almost any region of the body such as the volar wrist, hypothenar or thenar eminence, or from the foot.
Ideas
Patients and surgical techniques
A small FTSG was performed for patients who underwent free partial second toe pulp transfer reconstruction for fingertip defects between January 2019 to January 2020 who required additional pedicle coverage. Patient photographic consent was obtained in written form for all patients. This study was approved by the Institutional Review Board of Uijeongbu St. Mary’s Hospital (IRB No. UC21ZISI0132).
The shape and dimensions of the defect were measured under local or general anesthesia after the recipient finger was debrided until a healthy bed was exposed. After the free flap was harvested and inset according to previously discussed methods, any soft tissue defect overlying the anastomosed digital artery and donor artery was covered with a FTSG [1]. While an FTSG can be harvested virtually anywhere in the body given that it has enough redundant skin for tension-free closure, we preferred to harvest skin from the infra-malleolar region ipsilateral to the flap donor site, save for a single case. This area was chosen because it was in the same surgical field as the partial second toe pulp free flap, was a non-hair bearing location, and could avoid conspicuous scars. The donor site for case no. 2 was the hypothenar eminence of the ipsilateral hand because the patient requested ambulation early after the operation. The harvested skin was sutured to the margins of the defect using #5-0 nylon sutures, and then additional fixation was applied by spraying a fibrin sealant (Tisseel; Baxter Healthcare Corp., Deerfield, IL, USA) on the surrounding margins so that a thin layer of sealant connected and was overlying the graft and the adjacent skin [10]. This layer was not watertight, therefore allowed drainage of discharge or hematoma, and required ointment dressings to prevent desiccation.
Postoperative care
Dressings were changed daily using saline, ointment, and foam material with no additional compression applied to the graft. Both Mupirocin ointment (Esroban; JW Pharmaceutical Corp., Seoul, Korea) and recombinant human epithelial growth factor ointment (Easyef; Daewoong Pharmaceutical Corp., Seoul, Korea) were applied. The graft was lightly covered with a thin minimally adhesive foam dressing (Mepilex Lite; Mölnlycke Health Care, Gothenburg, Sweden).
Results
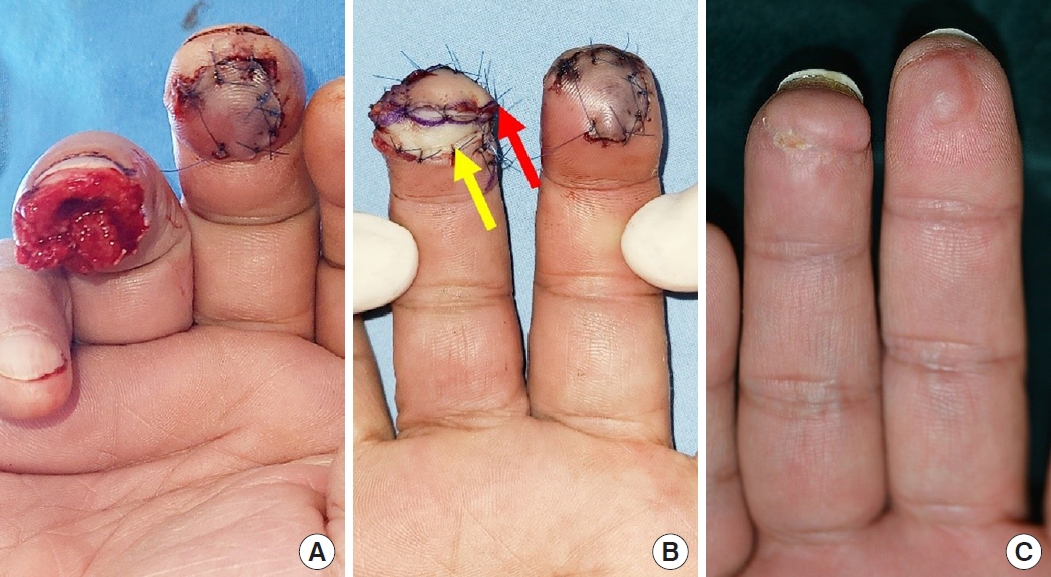
A total of seven patients were included in this study, two females and five males. Ages ranged from 42 to 63 years. Mean follow-up was 165±141 days. The demographics are summarized in Table 1. Each patient received a partial second toe pulp free flap for one digit. One male patient was a current smoker, one male patient was an ex-smoker, and the others were nonsmokers. Three patients were taking medication for hypertension, one person for diabetes mellitus. Five had experienced work-place related crushing injuries from industrial machinery, one sustained an amputation from farm work, and one person was injured by a heavy door. The average defect area was 3.78±1.98 cm2. The average area of the free flap was 2.39±1.03 cm2 and average graft area for the pedicle was 1.37±1.06 cm2. The flap survived without loss in all patients. Six of the grafts survived and were well-taken by the second week after surgery, but epithelial sloughing was seen after repeated hematoma collection was found in one patient (case no. 1) (Fig. 1). The graft healed during the following 2 weeks using recombinant human epithelial growth factor ointment dressings. Initially, the graft bulged out from the digit’s smooth contour, but as the flap became stable and swelling decreased, this volume irregularity normalized (case no. 1) (Fig. 2). By 8 weeks the texture and contour were almost identical to that of the surrounding digit skin (case no. 2) (Fig. 3). All donor sites healed by the second week after surgery when sutures were removed without disruption. Operative details are summarized in Table 2.
Discussion
The geometry of the digit forms the slimmest cylinder of the human body. Coverage of the anastomosis or pedicle is often required to prevent strangulation by local tissue. Skin grafts have often been used to provide shelter for the pedicle in free or pedicled flaps. Some authors have weighed against this option, deeming it endangering the vessels. STSGs have a thickness of 0.25 mm to 0.5 mm, barely providing any tissue volume, and therefore may seem quite fragile. However, Han and Min [9] have applied STSGs to overlie various flap pedicles of the body, and have found that they were more durable than previously asserted [9]. Their hypothesis is that the adventitia of the vessels were the optimal bed for graft take, supplying direct vascular ingrowth.
While the authors have experience applying STSGs to pedicles, muscles, or other areas of hand skin defects, we have found that harvesting the STSG and manipulating the thin graft during surgery is cumbersome. Harvesting a tiny STSG will require use of a small blade (such as the Humby dermatome or razor blade) which is hardly used in the modern operating room. Using a pneumatic dermatome, even the smallest blade will result in surplus harvest, unnecessarily increasing the donor area. Being depleted of most of the dermis, fixation requires gentle technique to prevent the graft from damage. Because the flap is usually well vascularized, oozing from the vicinity threatens loss of the thin graft during postoperative care. The FTSG, on the other hand, is easily harvested in any small dimension required, and does not necessitate use of the dermatome. Donor site closure results in elimination of any raw surface as in STSGs. The largest advantage is that FTSGs include a sturdy layer of dermis that provides structure for suture fixation and contributes to a thicker layer of coverage for the pedicle. Although this additional tissue may increase oxygen or nutrient demand, and together with the lack of compressive dressings be a cause for failure to take, we think that the abundance in vascularity just beneath the graft was the key factor that enabled stable tissue engraftment.
In the partial second toe pulp free flap, the digital nerves are anastomosed near the digital arteries, and therefore the fact that the graft will also be directly overlying the nerve should be taken into consideration. The fingertip is exposed to constant friction and pressure, and long-term durability comparison studies should be performed in the future.
This study is limited by its small sample size and lack of control group. Future large-scale studies comparing the FTSG with STSG to cover pedicles are warranted to discern which method is more optimal. However, our preliminary results suggest that the FTSG is a feasible option for coverage of the pedicle in free flap fingertip reconstruction.