Introduction
A keloid scar is an idiopathic outcome of collagen accumulation during the wound healing process [1,2]. Generally, it happens after trauma or surgery, and especially susceptible sites include the shoulder, chest wall, and ear. Treating a keloid scar is always challenging due to its tendency for recurrence [3,4].
The ear is one of the most common sites where keloid scars occur [5]. A keloid on the ear often results from ear-piercing, and intralesional injection of triamcinolone is known as the treatment of choice [6]. However, a keloid with a large volume cannot be easily reduced by intralesional injection alone. For efficient treatment, surgical excision is needed.
If a large keloid has a narrow stalk, it can be surgically removed by complete excision and primary closure. However, the same procedure is not applicable to a large keloid with a broad stalk. A large keloid with a broad stalk cannot easily be removed completely, as the diameter of the defect made by complete excision would be wide. The surgical goal for treating this should be debulking its volume rather than complete removal. A fillet flap using remnant scar tissue after debulking is a useful option for reconstructing a keloid on the ear, especially a large keloid with a broad stalk.
Methods
This study was conducted in conformity with the World Medical Association Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Hanyang University Guri Hospital (IRB No. 2022-03-028). The patients provided written informed consents for publication.
From April 2016 to June 2021, 24 cases of keloids on the ear were reconstructed using fillet flaps. Patient demographics, surgical outcomes, and keloid recurrences were recorded. There were four males and 20 females, with a mean age of 25.3 years (range, 13–50 years). All the patients had a large keloid with a broad stalk whose width was more than 1 cm.
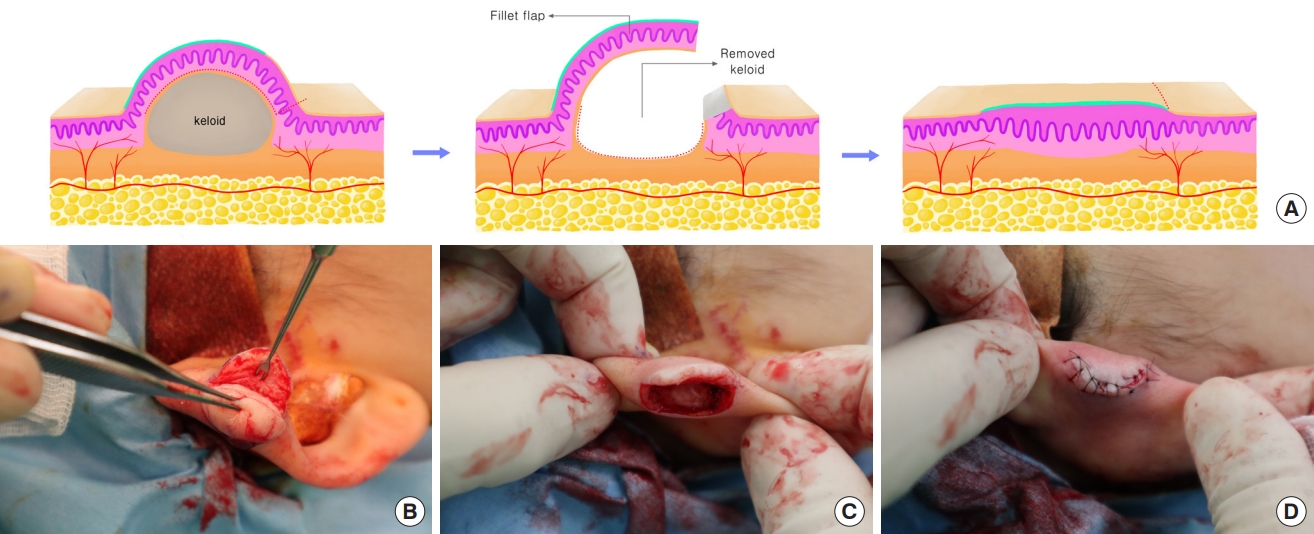
The operative procedure was performed under local anesthesia (2% lidocaine with epinephrine 1:80,000). The horizontal and vertical lengths of the keloid stalk were measured to estimate the dimension of the defect left after keloid excision. A round-shaped flap similar in size to the presumed defect size was designed on the surface of the keloid scar. The trapdoor-shaped flap was designed for the pedicle base to be placed on the more exposed side of the auricle so that the sutured site of the flap margin could be hidden in the relatively unexposed opposite area. The flap margin except the pedicle area was incised using a scalpel. All scar tissues including the fibrous keloid core were surgically removed except for the designed flap area consisting of a thin envelope of keloid. Electrocautery was used to separate the fillet flap from the keloid core with caution to preserve the subdermal plexus within the flap. The fillet flap was used to cover the defect left after keloid excision (Fig. 1). The thickness and dimensions of the flap were tailored to cover the defect without tension. The wound was closed with interrupted sutures and a pressure dressing was applied.
Patient follow-up was performed every month for at least 1 year postoperatively. During the first postoperative year, oral tranilast (a transforming growth factor-β suppressor) was administered to reduce the risk of recurrence. The patients were also educated to use silicone gel consistently on the surgery site. When keloid scar recurrence was observed, an intralesional injection of triamcinolone was performed.
Results
The 24 cases were composed of 19 keloids resulting from ear-piercing and five cases with other causes such as trauma and operative scars (Table 1). Four cases had experienced intralesional injections or surgical revisions before undergoing fillet flap surgery. All 24 cases were reconstructed with a fillet flap, and all flaps survived without any major problems. One case presented with a minor problem (wound dehiscence) but the wound healed successfully. In all cases, the contour and volume of the postoperative flap were flat enough that an initial injection of triamcinolone was not needed. However, in nine cases (38%), keloid recurrence was observed during the follow-up period, generally occurring within 3 months postoperatively. All recurred cases received triamcinolone injections, and the mean number of injections was 2.7. Among the nine recurred cases, one case showed a second recurrence 10 months after the first recurrence. Two more intralesional injections were needed for this case to make the recurred keloid flat.
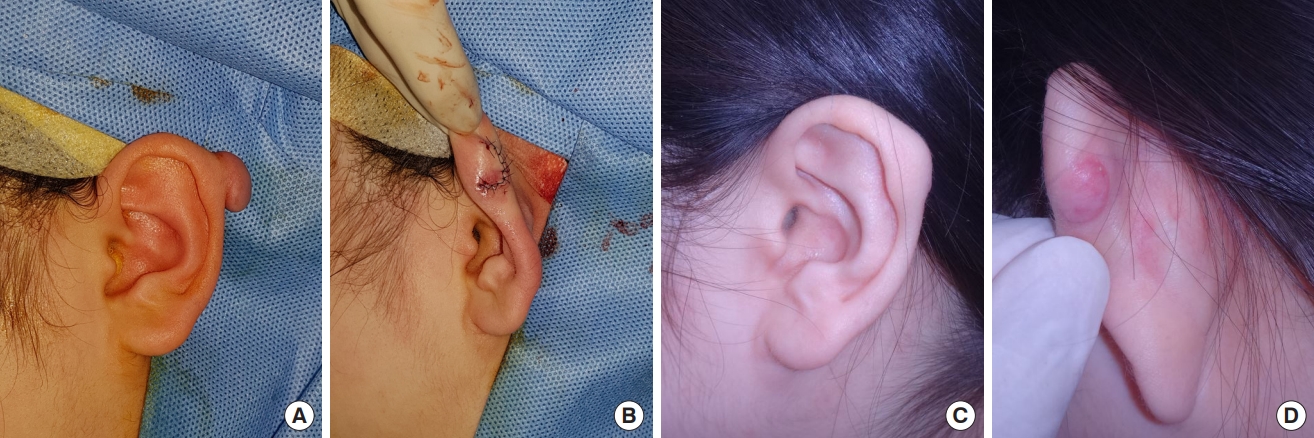
Case 1
A 21-year-old female patient presented with a keloid scar on her left earlobe (Fig. 2). The keloid appeared 2 months after her ear helix was pierced. The size of the keloid was 1.5×1.5×1 cm, which required surgical debulking and fillet flap coverage. The keloid was reconstructed with an appropriate contour, and no recurrence has been observed for 32 months of follow-up.
Case 2
A 41-year-old male patient presented with a keloid scar on his left earlobe, which had appeared after an abrasion injury left a scar which gradually grew (Fig. 3). The size of the keloid was 3×2.5×2 cm. Surgical debulking and fillet flap coverage were performed, and the keloid was reconstructed with a smooth contour and no distortion of the ear shape. There has been no recurrence of the keloid for 17 months of follow-up.
Case 3
A 20-year-old female patient presented with a keloid scar on her left ear helix (Fig. 4). The keloid appeared 2 months after the helix was pierced. The size of the keloid was 2×2×1 cm, and it was treated with surgical debulking and fillet flap coverage. At first, the postoperative contour was satisfactory and appropriate, but 3 months later protrusion of the operative site was observed. The recurrence required an intralesional injection of triamcinolone. The protrusion was solved with the injection and there has been no change during a follow-up period of 22 months.
Discussion
The goal of treating a keloid on the ear is to reduce its volume and make it flat. The treatment can be divided into non-surgical and surgical methods. The most commonly used non-surgical method is intralesional injection of triamcinolone, which is appropriate for small-volume scars. The surgical method is complete excision or debulking of the keloid, and this is appropriate for large-volume scars.
The exact method of surgical treatment can differ based on the stalk width of the keloid. When the stalk is narrow, complete excision and wound closure by approximation are possible. However, with a broader stalk, the surgical goal should be to debulk the scar volume rather than achieve complete excision. Excessive excision of a large auricular keloid with a broad stalk precludes the possibility of primary closure, as it leaves a wide defect. Furthermore, excessive approximation of the defect edges may result in distortion of the ear shape [7]. While partial wedge resection of a keloid may not disrupt the ear shape, it can leave too much remnant tissue of the scar, which can be a source of keloid recurrence. As a result, an appropriate surgical option should be the removal of as much keloid tissue as possible while preserving the shape of the ear.
The fillet flap is a local flap made from the surface of the keloid scar [8]. When excising scar tissue, a thin envelope of keloid scar can be left as a fillet flap. This enables the removal of more scar tissue than with wedge resection. In addition, covering the defect with a fillet flap can preserve the ear shape, as there is no need for approximation of the defect edges. The thickness and dimensions of the flap can be modified according to the size of the defect. The circulation of the flap is safe unless its thickness is extremely thin.
A drawback of the fillet flap when reconstructing an ear keloid is the possibility of keloid recurrence. Although the use of a filler flap permits more removal of scar tissue than that of wedge resection, this technique is still not free from keloid recurrence because the flap is still a part of the original keloid scar. Chong et al. [9], suggested that incomplete excision of keloid scar results in a 25% recurrence rate, whereas our study showed a 38% recurrence rate. This is lower than the recurrence rate (44%) of another study for the reconstruction of auricular keloid scar using the fillet flap [8]. However, higher recurrence rates for fillet flap coverage compared to complete excision and primary closure are still controversial; Chuan et al. [10], suggested that the recurrence rate of keloids reconstructed with a fillet flap is not statistically higher than that of keloids reconstructed with primary closure. They insisted that their results of using the fillet flap provided reassurance against the concern that this method might cause higher recurrence rates because of the risk of remnant keloid tissue in the flap.
Postoperative care is also important in reducing the recurrence rate [11]. The literature introduces various options such as oral agents, silicone products, radiotherapy, and pressure therapy using magnets [12-15]. We administered oral tranilast and silicone gel postoperatively for 12 months to our patients. This may be a factor that lowered the recurrence rate in this study compared to that of Kim et al. [8]. However, the most important thing is routine observation of the scar. Routine follow-up every month for the first 12 months is essential as this is a critical period for scar formation in the wound healing process. Patients should be educated to visit the clinic whenever recurrence is observed, even after the first postoperative 12 months. Recurrence generally occurs within the first 3 postoperative months but can be delayed for up to several years [16]. If recurrence is observed, an intralesional injection of triamcinolone should be considered before the keloid becomes rapidly enlarged.
The literature also introduces combination therapy for ear keloids using the fillet flap and adjuvant triamcinolone injection [4,7]. These studies performed intra-flap injection of triamcinolone intraoperatively or just after the surgery. The injection was also postoperatively performed routinely multiple times in every case. These studies generally show a low recurrence rate from 0 to 10%, whereas the recurrence rate after keloid excision without triamcinolone injection is more than 60% [17]. However, a drawback of the combination therapy is that every patient receives multiple steroid injections regardless of recurrence. This regimen bears the possibility of steroid injection-induced complications such as telangiectasia or poor wound healing in every patient. On the other hand, our study only administered triamcinolone to the patients who displayed keloid recurrence. Although our recurrence rate was higher than that of the combination therapy, our regimen avoids the risk of steroid injection in patients who present a normal course of wound healing and scarring.
Reconstruction of a keloid scar on the ear using the fillet flap aims to provide a small and flat scar condition by removing as much scar tissue as possible, especially in the case of a large keloid with a broad stalk. The final goal of the surgery is not the complete removal of the scar but making the scar flat enough for intralesional injection when recurrence is observed. Although this method of debulking and coverage with a fillet flap does not guarantee a cessation of recurrence, it is a useful surgical option.