Introduction
Penetrating injuries of the face are frequently encountered in the emergency room (ER). Although not as common as other injuries, deep injuries and retained foreign bodies due to sharp objects can cause severe complications [1]. In such patients, detection of the retained foreign body is the first obstacle faced by a physician. In the case of penetrating injury caused by long wooden objects such as disposable wooden chopsticks, it is difficult to identify foreign substances in the face because of the small opening.
If a remaining foreign body is suspected, plain radiography is the first diagnostic tool of choice. However, only radiopaque materials can be detected by radiography. Therefore, ultrasonography is considered a practical first-line procedure for detecting foreign bodies [2]. It is an easy tool to use and handle; however, detection of a small wooden material on ultrasonography relies heavily on the experience of the operator [3]. Computed tomography (CT) is considered another useful tool for detecting foreign bodies; however, it is difficult to detect a wooden material on CT [4]. Limited studies have demonstrated the appropriate CT settings to distinguish wooden foreign bodies from the surrounding environments and tissues [5,6].
Here, we present a case to highlight the importance of thorough examination and diagnosis of retained foreign bodies and how their sequelae can easily be mistaken as bite wound infections. This study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-EXP-2022-025). The patient provided informed consent for the publication of her clinical and radiological data.
Case
A 47-year-old woman visited the ER in a drunken state presenting a 0.5-cm entry wound on the left temporal area. According to the patient, she was attacked by another individual after an argument. During the incident, the injury had been caused by a wooden chopstick that had already been used for eating. The skin-penetrating chopstick was then removed from the site. No other specific findings were observed on frontal plane radiographs of the skull. The wound was primarily closed after being irrigated several times with normal saline and the patient was discharged from the ER. Additionally, amoxicillinclavulanate (875/125 mg) was prescribed to be taken twice daily for 4 days. The patient was advised to visit the outpatient clinic daily for povidone-iodine-soaked gauze dressings but did not appear for follow-up. Approximately 14 days later, the patient revisited the ER complaining of extensive swelling and erythema in the left cheek (Fig. 1).
Fig. 1.
Clinical photograph showing erythematous swelling on the left cheek. The scar is present on the left temple area.

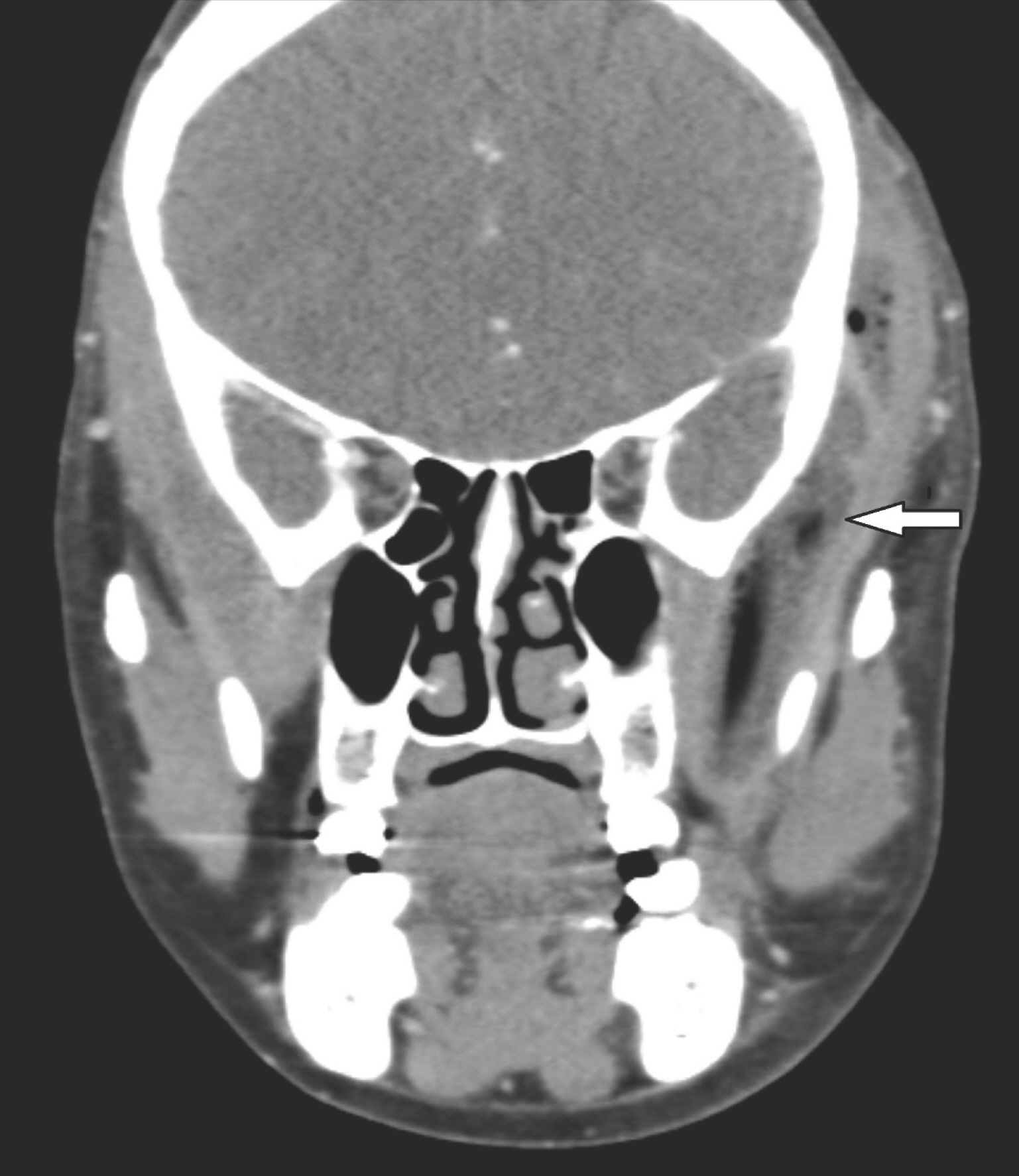
Initial blood tests revealed elevated C-reactive protein levels and a borderline electrolyte imbalance. Enhanced facial CT indicated an abscess cavity formation in the left masticator space and adjacent parapharyngeal space (Fig. 2). The patient was immediately transferred to the operating room for surgical drainage under local anesthesia. Incision and drainage were performed on the previous scar in the left temporal area, and additionally in the left lower gingivobuccal area (Fig. 3). A sufficiently long catheter was placed under the temporalis plane, which extended into the lateral pterygoid muscle. The exudate from the wound was used for Gram staining and bacterial culture. Gram staining revealed Gram-positive cocci and bacilli, and Staphylococcus epidermidis was isolated from the cultures, which led us to believe that oral flora had colonized the wound. Since the patient had used the chopsticks before the penetration injury, the wound was treated as a human bite.
Fig. 3.
Surgical management was done under general anesthesia. (A) Incisional drainage is performed in the left temporal area to approach the masticator space. (B) An additional incision is made on the left lower gingivobuccal area to approach the lateral pharyngeal space intraorally.

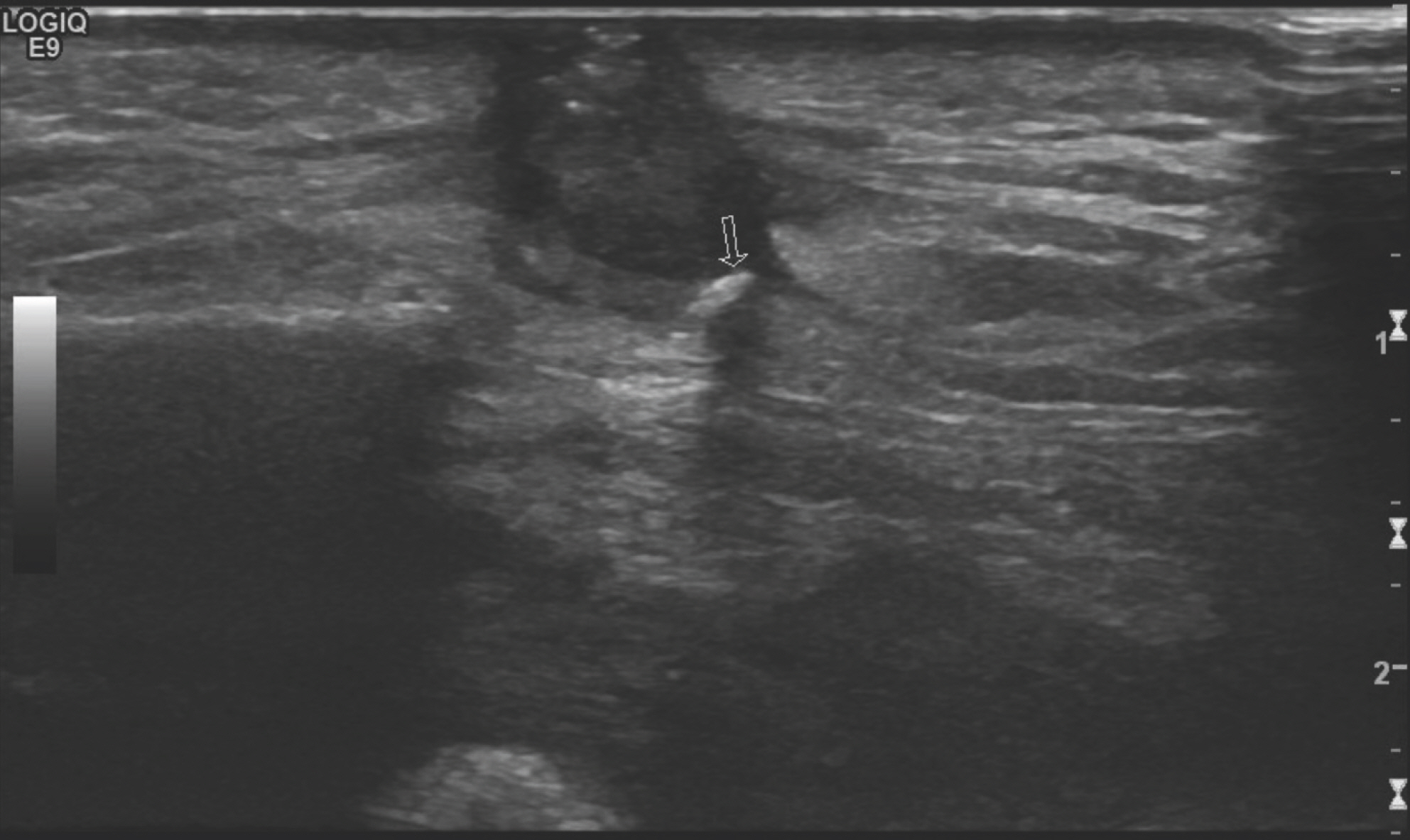
In addition to amoxicillinclavulanate, metronidazole (500 mg, three times daily) was administered to cover anaerobic bacteria and the wound was irrigated in the operating room daily for 14 days. The symptoms and signs of infection seemed to regress for the first 10 days. However, the characteristics of the fluid discharge then aggravated and the symptoms wors-ened, which led us to suspect the presence of a remaining foreign body. Ultrasound examination was performed to locate any remaining foreign bodies, which displayed an abscess pocket containing a foreign body in the left cheek (Fig. 4). Under general anesthesia, extensive and thorough exploration was performed immediately under the temporalis plane. Several fragments of the wooden chopstick, amounting to a total length of approximately 11 cm, were found and removed (Fig. 5).
The patient did not develop any further symptoms or complications after surgery. The wound healed well by secondary intention.
Discussion
Penetrating injury to the facial area is one of the most common types of injury observed in the ER. However, treating infections caused by retained foreign bodies after such penetrating injuries can be a difficult task. The likelihood of developing infection varies according to factors such as age, sex, mechanism and location of injury, and underlying diseases [7]. According to various reports, organic materials such as wood tend to have more potential for inflammation than metallic materials because they provide a favorable environment for microbial growth [8].
Chopsticks are the most commonly used cutlery in Asia, and wooden chopsticks are widely used owing to their convenience. However, disposable chopsticks are sometimes poorly manufactured and can be a medium for bacterial growth [9]. Therefore, if a chopstick is retained in the human body, it can easily become a source of infection. Penetration with chopsticks often occurs after they have already been used to put food in one's mouth, implying that they are contaminated by oral bacteria. Once wound infection progresses, it is difficult to determine whether it was caused by oral bacteria or any remaining foreign bodies such as wooden chopstick fragments.
The diagnosis of indwelling wooden materials of any kind is frequently a challenging matter. Plain radiography is a routinely used imaging technique on patient presentation to the ER. However, wood is usually radiolucent and cannot be detected by simple radiography. Ultrasonography is mainly used to detect foreign bodies embedded in soft tissue [10]. However, ultrasound does not always visualize underlying foreign bodies if the operator is inexperienced or the fragments are surrounded by body fluids such as pus or blood [11]. In our case, the foreign material was detected on follow-up ultraso-nography performed on the left cheek abscess.
On CT scans, unlike metallic materials, wooden foreign bodies appear hypodense and are easily overlooked because of their similarity to air, easily leading to a misdiagnosis [12]. Moreover, inaccurate recollections or statements of how the patient was injured compounded with an absence of prominent symptoms can cloud a physician's judgment. If CT findings do not show a clear diagnosis when symptoms aggravate, performing a magnetic resonance imaging (MRI) could be an alternative choice in making a diagnosis, for wooden material easily appears hypodense on both T1 and T2-weighted images [13]. However, ordering an MRI scan on a patient without emergent symptoms can easily be perceived as an overtreatment, which most patients would like to avoid. Therefore, to effectively detect wooden foreign bodies on CT, several authors have used a wide window level width setting of approximately 1,000 HU (Hounsfield unit) and –500 HU. This particular setting can help distinguish wooden material once air forms around it [13,14]. However, it is not applicable in every situation because wood tends to become denser once it absorbs more water and blood. Nonetheless, CT is the best tool for diagnosing a retained wooden foreign body, in terms of both time and cost, and physicians should always keep in mind the possibility of retained foreign bodies and thoroughly check CT scans for such signs.
Masticator space abscesses are usually derived from odonto-genic infections caused by bacteria inhabiting the oral cavity. The traditional approach of draining the abscess can be performed via a transcervical incision made under the subman-dibular gland. If the abscess is located medial to the main artery, incision and drainage can be performed transorally [15].
Limitations of this study include the fact that quicker and more specific diagnostic tools should have been used when the abscess had not resolved and when the patient first presented at the ER, various modes of CT scans could have been done for more thorough investigation of the wound.
The detection of wooden foreign bodies is a challenging clinical problem. When such a penetration injury is evaluated, it is important to identify any wooden foreign bodies using various imaging studies. Furthermore, it should be kept in mind that penetration injuries caused by wooden chopsticks usually occur after the chopsticks have been introduced inside the oral cavity, increasing the likelihood of wound infections.