Introduction
Morel-Lavallee (ML) lesions were first reported by a French physician in 1863 after a post-traumatic fluid collection occurred after a patient fell from a train [1]. ML lesions are caused by the accumulation of hemolymphatic fluid in a hypovascular suprafacial space that is formed following a trauma event. Various terms are used to refer to ML lesions, including post-traumatic pseudocyst, post-traumatic soft tissue cyst, closed internal degloving lesion, and chronic expanding hematoma; it may occur anywhere from head to toe [2]. Vanhegan et al. [3] reported the rate of occurrence of ML through several case reviews as follows: greater trochanter or hip, 30.4%; thigh, 20.1%; pelvis, 18.6%; knee, 15.7%; gluteal region, 6.4%; lumbosacral region, 3.4%; abdominal wall, 1.5 %; calf or lower leg, 1.5%; head, 0.5%; and others, 2.0%. ML lesions are not commonly encountered, and depending on the site of involvement, their diagnosis may be delayed, or they may be misdiagnosed as bursitis, sarcoma, lipoma, or other soft tissue masses [3,4]. Chronic ML lesions form hematomas, which increase the chances of infection; capsule formation makes surgical treatment inevitable [5]. Therefore, accurate diagnosis and prompt treatment are essential in ML lesions.
ML lesions can be diagnosed if clinical features, such as painful fluctuant swelling, are observed in a patient with a history of trauma, and imaging features of ML lesions are confirmed through ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI). Once diagnosed, treatment strategies, such as compressive dressings, sclerotherapy, and surgical intervention can be established, considering the time of occurrence, range, and underlying condition of the wound [6].
The purpose of this case report is to introduce an effectively treated case using negative pressure wound therapy (NPWT), especially the PICO system (Smith & Nephew, London, UK), which provides a convenient disposable device, for acute ML lesions in the sacrum region. The study was approved by the Institutional Review Board of Chosun University Hospital (IRB No. 2021-12-011), and the patient provided written informed consent for the publication and the use of his images.
Case
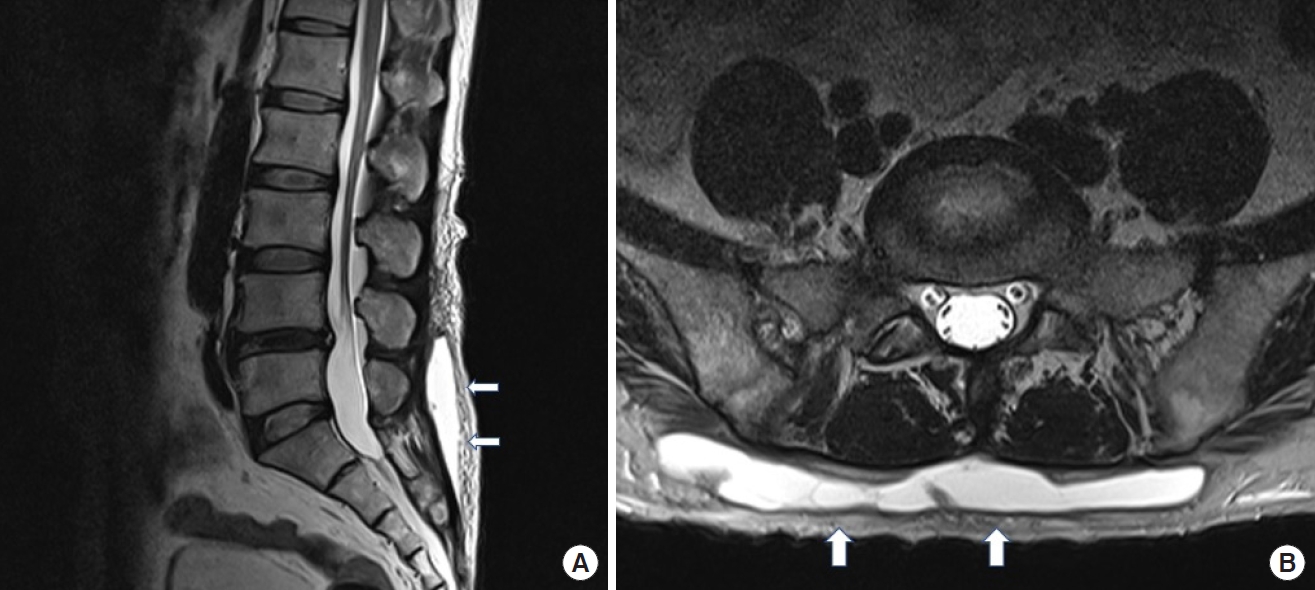
A 51-year-old man with no other underlying disease visited our clinic with fluctuating swelling in the sacral area. The patient had a history of trauma in which he had fallen from a height of 3 m 3 weeks earlier. On physical examination, a fluctuating hump was observed in the sacral area without any specific signs of infection such as erythema. The patient complained of numbness when the involved area was touched and mild pain when pressed. For further evaluation, a pelvic MRI was performed, confirming that a high signal intensity was observed at the suprafascial layer of the patient’s lower back in an area of approximately 15×8 cm (Fig. 1). These MRI findings indicated prominent fluid collection without capsule formation, and together with the patient’s previous history of trauma, identified the lesion as an acute ML lesion. As the patient refused inpatient treatment for personal reasons, we planned non-surgical conservative treatment with the patient visiting our outpatient clinic every 3 days.
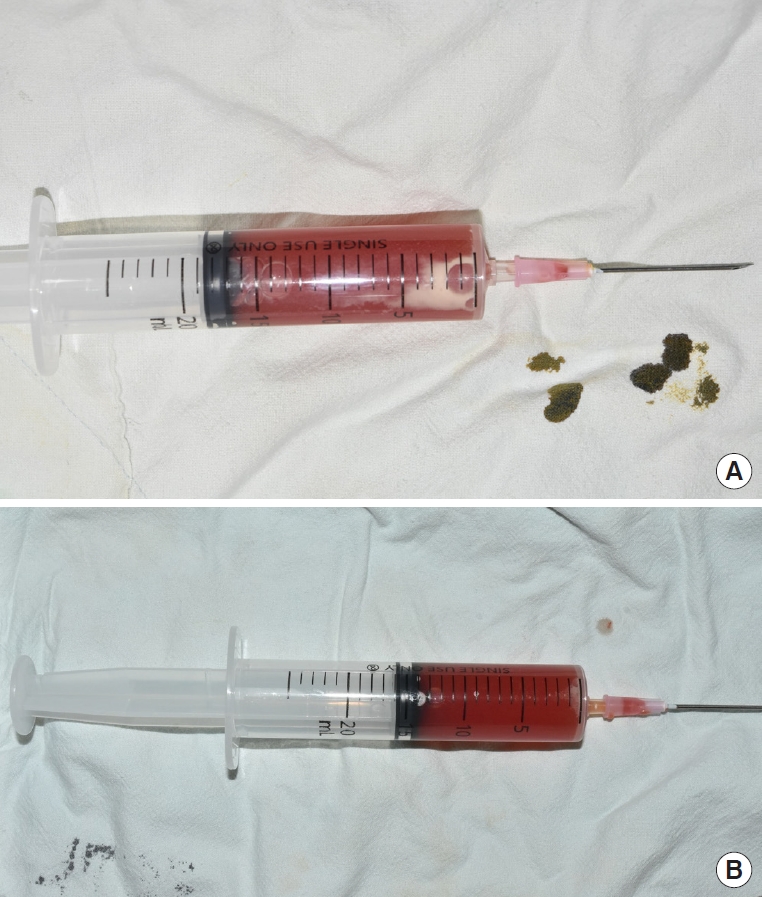
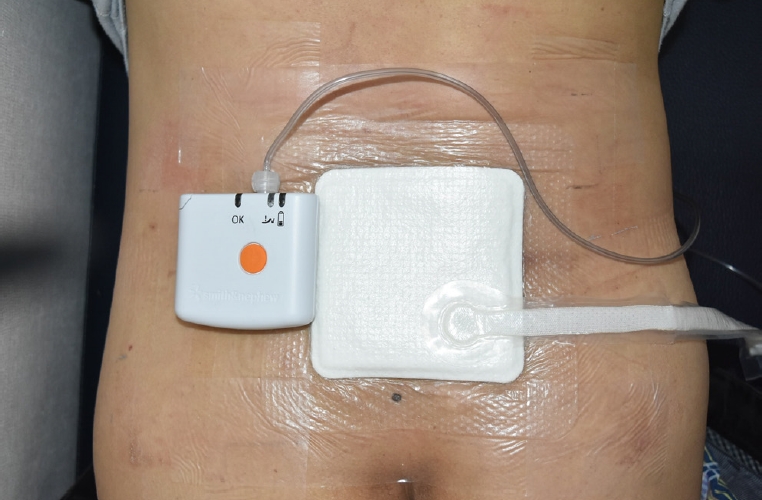
A total of 40 mL of serosanguineous fluid was drained by needle aspiration during the first visit, and compression dressing was performed upon the involved area using gauze and elastic bandages (Fig. 2). Bacterial culture tests of the drained fluid confirmed that there were no bacteria. Three days later, 30 mL of serosanguineous fluid was drained by needle aspiration. Next, 15 mL was drained between follow-ups; 15 mL was drained again three days later, and the amount of drainage remained the same. Because the patient had to bend and straighten at the waist constantly for occupational reasons, it was considered that the previous treatment was no longer effective. Considering the patient’s movement, we changed the treatment plan and used PICO after performing needle aspiration on the fluid collection site (Fig. 3). PICO application was performed every three days. After applying PICO, the amount of drainage during needle aspiration continued to decrease during follow-up. On the 3rd day after the first PICO application, 14 mL of fluid was aspirated, and 13 mL was drained after the second application. However, after the third PICO application, the amount of aspiration decreased to 8 mL, and afterwards, it was confirmed that the amount gradually decreased to 4 mL and then to 2 mL. Since the first PICO application, there were a total of six applications over the course of 3 weeks, and fluctuating swelling was no longer observed on needle aspiration and physical examination. The patient did not complain during the application of the single-use portable NPWT device (PICO). On a visit to our clinic approximately 1 year later, it was confirmed that the patient’s condition and wound site were stable without any special findings.
Discussion
ML lesions are rare post-traumatic closed degloving injuries that occur when the hypodermis separates from the underlying fascia due to an injury caused by a blunt or shearing force [1]. The most common locations of these injuries are the greater trochanter, hip, and thigh, following pelvic trauma. Other frequent areas include the knee and arm [7]. There have been reports of rare cases occurring after procedures, such as liposuction [1,7]. Most patients present with a history of trauma having occurred several weeks to months before and complaints of discomfort caused by nonspecific fluctuating masslike lesions of various sizes. If the lesion is left untreated for an extended period, the skin on the involved area may show discoloration, hyperpigmentation, or necrotic changes [7,8]. The diagnosis of ML lesions requires imaging tests along with these clinical findings. Ultrasonography, CT, and MRI are used, among which MRI is the most effective imaging tool. This is because MRI can easily assess three-dimensional anatomical structures through several sections and is excellent for diagnosing soft tissue diseases and masses that require differential diagnoses. In addition, by differentiating acute and chronic lesions through a difference in signal intensity, capsule formation requiring surgery can also be easily detected [8,9].
Although the treatment of ML lesions has not been clearly established, several studies recommend developing a treatment plan according to the patient’s clinical situation. Important clinical questions include the following: (1) has it been more than 3 weeks since the injury?; (2) are there any symptoms?; (3) is there a fracture, infection, or necrosis at the injured site?; (4) is the fluid collection >50 mL?; and (5) does radiologic examination show prominent capsule formation? [4,8].
In many cases, surgical treatment is required, and open debridement and closure are mainly performed. In some cases, sclerodesis is performed using doxycycline, talc, alcohol, bleomycin, or tetracycline [8,10]. Patients who can try conservative treatment first are those with a fluid collection of <50 mL without prominent capsule formation upon radiologic examination within 3 weeks after injury. Harma et al. [11] reported that acute lesions without any infections or necrosis were healed only with conservative management after an average of 6.8±3.96 weeks.
In this case, the fluid amount on the initial needle aspiration was 40 mL, and compression was performed using gauze and elastic bandages. Subsequently, regular aspiration and compressive dressing were performed. However, as the injury was in the sacral area, it was difficult to maintain the compression dressing during the patient’s daily routine because he mostly worked in a squatting position. The patient also preferred outpatient treatment to inpatient treatment, prompting us to plan for conservative treatment instead of surgery. Even after continuous posture change, PICO maintained a close attachment to the wound site. Therefore, the single-use portable NPWT device (PICO) can be considered a suitable treatment method for such patients.
Applying NPWT to closed incisions has benefits including earlier cessation of wound drainage and reduced rates of dehiscence and infection [12]. NPWT decreases lateral and shear stress at the closed incision, bolsters appositional forces at the wound, and increases lymph clearance with reduced formation of hematomas and seromas [13]. In particular, the PICO device is easy to operate, and most importantly, it is a small and canister-free device that gives less discomfort in the patient’s daily life. In addition, it delivers –80 mmHg negative pressure in a continuous pattern [14,15].
If the diagnosis of ML lesions or appropriate treatment is delayed, the collected fluid is retained, and capsule formation may occur. In most cases, surgical treatment is required for a complete cure and avoidance of infection. Therefore, a rapid and accurate differential diagnosis of ML lesions is important. During conservative treatment, if classic compressive therapy is difficult, the single-use portable NPWT device (PICO) can help maintain the compressive effect.