Introduction
Calcinosis cutis is a very rare disease characterized by normal serum calcium levels with high amounts of cutaneous and subcutaneous insoluble calcium salt deposit [1]. There are five types of calcinosis cutis: dystrophic, metastatic, idiopathic or iatrogenic calcification, and calciphylaxis [2]. The dystrophic type is mostly caused by damage of, or abnormalities in, local tissue, whereas the metastatic type is caused by abnormal calcium and phosphorus metabolism. The idiopathic type occurs without any tissue damage, and the iatrogenic type usually occurs after intravenous calcium or para-aminosalicylic acid treatment. Calciphylaxis is related to vasculopathy caused by ischemia or frank tissue infarction [3]. Moreover, calciphylaxis is mainly diagnosed in end stage kidney disease patients, due to the presence of arterial calcification [4].
Dystrophic calcification, the most common type of calcinosis cutis, is linked to various conditions such as connective tissue diseases, inherited disorders, cutaneous neoplasm, infection, radiation, and trauma [3,4]. In general, dystrophic calcinosis cutis appears many years after the onset of the underlying conditions described above [5].
The pathophysiology of calcinosis cutis remains unclear, and diagnosis is difficult in the absence of other symptoms such as ulcers or other comorbidities. Diagnoses are typically made based on the patient’s clinical features, blood test results, and tissue biopsy results. A standardized treatment is yet to be established; however, there are clinical reports using antibiotics, calcium channel blockers, hyperbaric oxygen (HBO), intralesional corticosteroids, and surgical intervention [4].
Herein, we report a case of a patient who visited our clinic for a chronic wound with a suspected large foreign body under the wound. The patient was diagnosed with calcinosis cutis after surgical removal of the suspected foreign body. We obtained written informed consent from the patient. The study was approved by the Institutional Review Board of Kosin University Gospel Hospital (IRB No. KUGH-2020-09-007) and performed in accordance with the principles of the Declaration of Helsinki.
Case
A 69-year-old woman visited our hospital with a main complaint of an ulcerative wound on the right posterior calf. The patient had an unremarkable medical history with no underlying diseases, except for a right posterior calf burn scar from 10 years ago. Prior to the current hospital visit, the patient was treated at an oriental clinic 9 months ago, following a dog bite injury on the existing burn site. However, she visited our hospital because the dog bite site was not healing well for 10 months despite treatment at the oriental clinic.
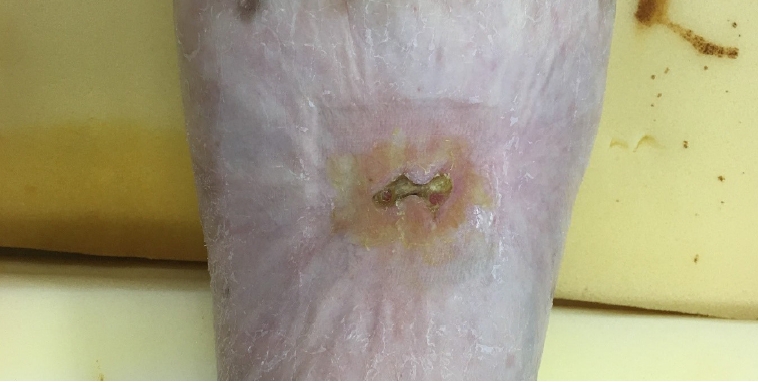
At the time of presentation, we observed an open chronic wound of 2.3×1.5 cm with purulent discharge, which we considered the dog bite wound. We performed a bacteria culture test of the discharge; however, no bacteria were identified. During physical examination, we palpated a hard mass under the wound which was larger than the wound, and we suspected it to be a large foreign body (Fig. 1). Consequently, an X-ray and lower extremity computed tomography (CT) were performed to evaluate the suspected foreign body. A thin radiopaque plate-like material was detected in the posterior calf by X-ray, and the presence of the foreign body was confirmed by CT (Fig. 2).
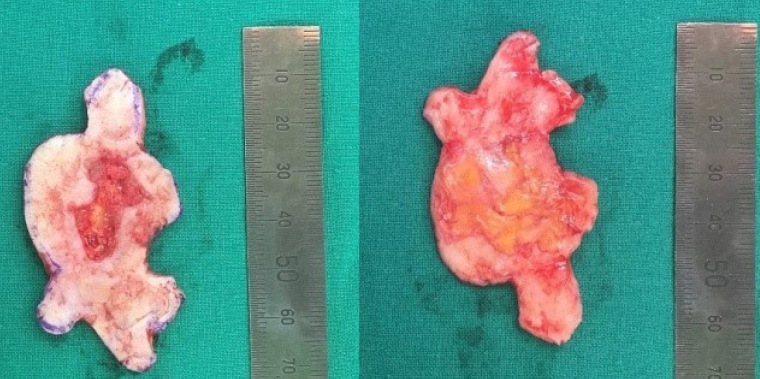
We performed a biopsy by resecting 6×4 cm of skin, containing the ulcer and the mass (Fig. 3). Postoperative split-thickness skin grafting was performed on the excision area.
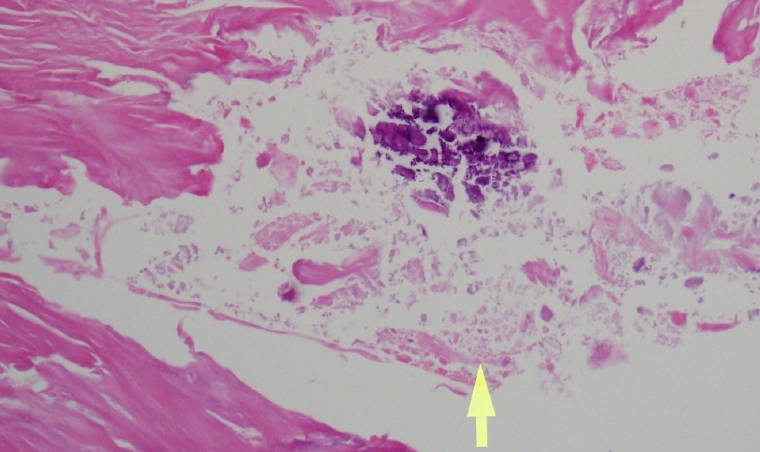
The graft site healed, and the patient recovered without any complications. Hematoxylin and eosin staining of the biopsy specimen led to a diagnosis of calcinosis cutis (Fig. 4). No calcified lesions were identified in a follow-up X-ray, and the patient reported no recurrences during a 2-year follow-up period (Fig. 5).
Discussion
Calcinosis cutis is a disease caused by abnormal dermal and hypodermal deposition of calcium salts. The clinical features of calcinosis cutis are variable and appear in the form of firm, painless, white, yellowish or flesh-colored papules, plaques, or nodules [6]. Non-healing ulcers are also a non-specific symptom that can occur in all types of calcinosis cutis [3].
The dystrophic type, the most common type of calcinosis cutis, is caused by local tissue injury or abnormalities. It is presumed that an increase in the alkalinity of necrotic tissue leads to calcium salt precipitation [3,7]. In this case, the patient was admitted because of a non-healing chronic ulcer with a suspected large foreign body. However, the biopsy result identified the foreign body as calcinosis cutis, and taking into account the patient’s burn history, the diagnosis was dystrophic type calcinosis cutis.
Whatever the mechanism or type of calcinosis cutis, treatment is always challenging. Small calcified deposits or larger localized lesions can be successfully treated with surgical excision. However, extended calcinosis usually requires systemic treatment, such as the use of probenecid, diltiazem, aluminum hydroxide, bisphosphonate, or HBO therapy for several months [4,8]. Probenecid, aluminum hydroxide, diltiazem, and bisphosphonate can be used to control serum calcium and phosphate levels and to reduce the size of the calcification [8]. HBO treatment can increase tissue pO2 levels while reducing tissue edema and ischemia, and inhibit bacterial growth by enhancing angiogenesis. Reducing ischemia by HBO treatment can prevent the development of ischemic eschar, the major cause of calcification formation in calcinosis cutis. HBO is therefore recommended particularly for inoperable calcinosis cutis patients [4,9]. However, the shortcoming of HBO therapy for calcinosis cutis is that it can only promote healing of the wound without fundamentally curing the disease. Additional treatment options including wound care and correction of hyperphosphatemia are also required.
Among the five types of calcinosis cutis, dystrophic calcinosis cutis is mainly related to autoimmune disease of the connective tissue. However, because it is difficult to treat such diseases, the primary goal of treatment regimens for dystrophic calcinosis cutis is to relieve symptoms and alleviate functional limitations [10].
Patients with trauma-induced calcinosis cutis are not common; however, Larralde et al. [11] reported a case of a patient in whom calcinosis cutis resulted from inguinal fold trauma. In the report, the authors presumed that the tissue injury that caused calcinosis cutis was postoperative inflammation or inflammatory reaction to suture material as a foreign body [11]. In our case, because we initially had limited information from the patient, and considering some reports about complications after foreign body implantation at oriental clinics, we initially presumed the large hard mass to be a foreign body implanted at the local oriental clinic and the un-healing ulcer a result of foreign body infection [12]. However, after the negative bacteria culture, we diagnosed the mass as dystrophic calcinosis cutis, based on pathology examination and trauma history.
While dystrophic calcinosis cutis can occur at the site of a burn scar, the time interval between the burn injury and onset of calcification onset remains very variable. Reiter et al. [3] demonstrated that calcification might occur many years or decades after the injury. Based on literature review, the shortest period of onset was 1.5 years after a pencil tip trauma and the longest period was a report from Heim et al. [13] that occurred 31 years after an injury from boiling water. Therefore, it is difficult to estimate the time from trauma to onset of calcinosis cutis. In our patient, the dog bite injury was too recent to be considered the cause of calcification. Also, the calcification was widely spread under the burn scar, and the area of calcification was wider than that of the dog bite injury. Based on previous case reports and considering the patient’s clinical presentations, the cause of calcinosis cutis in the current case was most likely the burn injury.
Meanwhile, there is heterotopic ossification (HO) which develops similar symptoms after burns or trauma [14]. HO is a disease wherein bone formation occurs in soft tissue, and being clinically similar to calcinosis cutis, it is difficult to differentiate by standard imaging investigations. However, HO can be diagnosed histologically using biopsy. While abnormal bone formation is observed in HO, only calcium deposition is observed in calcinosis cutis. Therefore, we diagnosed our patient with calcinosis cutis, based on the presence of calcium deposition in the dermis on histopathological examination.
According to literature, the average size of calcinosis cutis is relatively small [15]. However, in our case, the patient had only one lesion, and it was relatively large (6×4 cm). This was one of the reasons why the initial presumptive diagnosis was a foreign body rather then calcinosis cutis.
Calcinosis cutis is a very rare disease, and therefore, a subcutaneous hard mass can be easily misdiagnosed as a foreign body or another disorder. Therefore, it is important to perform a biopsy if a non-healing ulcer or hard mass is identified in a patient with a history of trauma, burn, or systemic disease.