Introduction
Hot-melt adhesives are applied with glue guns, which are frequently used by the general public. But high-pressure injection injuries associated with hot-melt adhesives are very rare and occur mainly in industrial workers. High-pressure injection injuries are generally underestimated because the patients tend to not complain much initially and because their clinical manifestations are in small skin lesions [1,2]. Such underestimation delays the treatment when early surgical debridement of foreign bodies is important in high-pressure injection injuries. If the foreign material is a hot-melt adhesive, it becomes more difficult to remove from the small wound opening because the material solidifies within.
Contact burns caused by hot-melt adhesives have been evaluated in some studies. There are also case reports related to high-pressure injection injuries, but most of them are related to grease, paint and hydraulic fluid. We present a case wherein a hot-melt adhesive was injected into a finger with a high-pressure industrial glue gun. The aim of this case report is to highlight the damage associated with high-pressure hot-melt adhesive injection injuries, which we believe is not sufficiently estimated by the naked eye. The study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Case
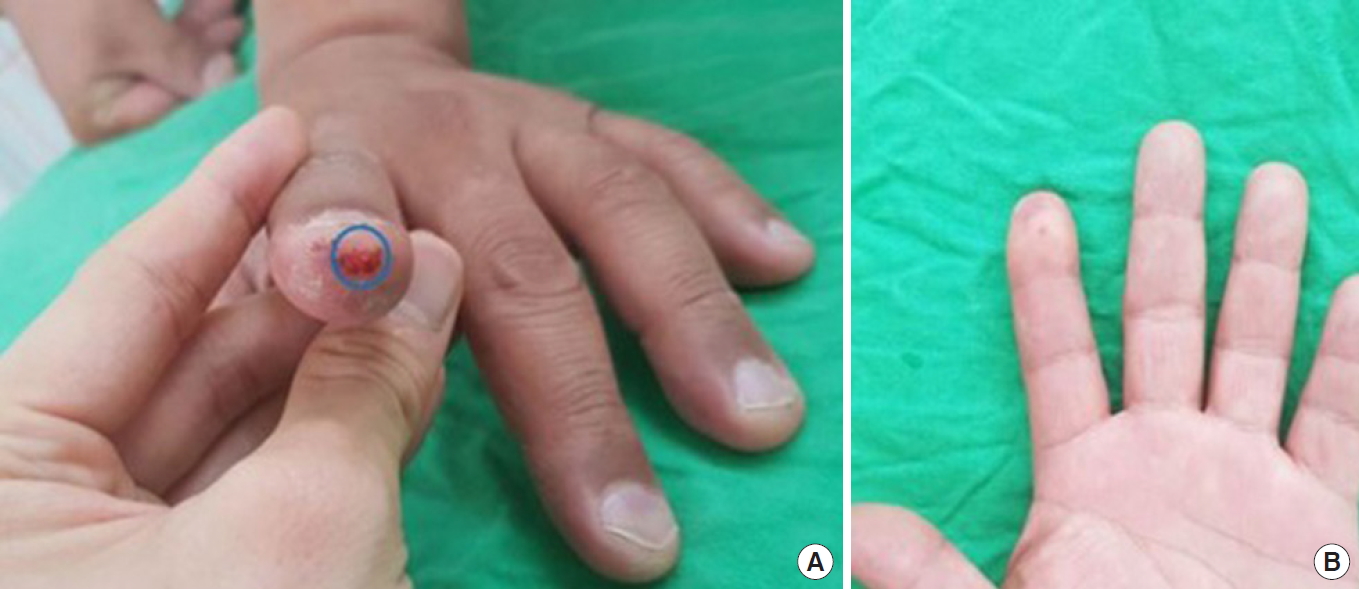
A 45-year-old man visited our department of emergency medicine with a high-pressure hot-melt adhesive injection injury on his left index finger. He had no specific medical history. When he first visited the emergency room, there were no unusual symptoms except for a tiny opening on the fingertip, mild swelling and erythema of the distal phalanx, and mild tenderness. Finger circulation (examined by using a Doppler device and capillary refill time) and sensation were found to be intact, and movement restrictions were not observed in any direction. Burns were not obviously observed either (Fig. 1). Because the patient mentioned that the injected material was industrial hot-melt adhesive, copious saline irrigation was performed. Also, intravenous antibiotics and tetanus prophylaxis were given in the emergency department. Attempts to squeeze the injured finger resulted in no excretion. Because early surgical debridement of foreign bodies is important in high-pressure injection injuries, we recommended surgical treatment and explained the possibility of amputation. But the patient refused any surgical treatment and hospitalization. After applying a dressing of wet gauze and antibiotic ointment, he was discharged and instructed to visit the outpatient department the next day for follow-up.
Four days after discharge, which was later than the scheduled date, he visited the hospital, and necrosis was observed at the fingertip to volar side of the distal phalanx when the dressing was opened (Fig. 2). There was no sign of infection, and the erythrocyte sedimentation rate and C-reactive protein level were within the normal ranges. Furthermore, no peculiar findings like fractures or foreign bodies were observed on a simple X-ray (Fig. 3).
One day later, necrosis did not progress, and demarcation was obvious. Surgery was performed to excise the necrotic tissue and remove hot-melt adhesive foreign bodies. Because a digital block can cause swelling and decrease perfusion, surgery was performed under a brachial plexus block [3]. Incisions were made along the necrotic tissue boundaries. Using a surgical microscope, necrotic skin and partial fat necrosis in the superficial part of the pulp were removed, and very small amounts of opaque foreign bodies were also removed. After a large amount of irrigation, the remaining tissue was closed with sutures (Fig. 4).
After the surgery, treatment consisted of intravenous antibiotic administration, and a povidone-iodine-soaked gauze dressing was applied without compression. Steroids and anticoagulants were not used because the possibility of vascular compromise was considered to be low, and also because the use of steroids is controversial and does not demonstrate a definite advantage in reducing the rate of amputation [1].
After the surgery, the patient was discharged on the same day, and he returned for wound dressing on the first postoperative day. Although no infectious signs were observed, there was a moderate amount of serous discharge from the wound. He was treated with povidone-iodine-soaked gauze dressing and oral antibiotics to prevent infection. Subsequently, he visited the outpatient clinic every other day povidone-iodine-soaked gauze dressing. Still there was a moderate amount of discharge from the wound for 7 days after the surgery (Fig. 5). Serous discharge without malodor was observed and wound cultures did not show any bacteria. As the discharge gradually decreased thereafter, the dressing method was changed to a foam with antibiotic ointment dressing and oral antibiotics were also discontinued. Three weeks after the operation, there was no discharge and the wound was nearly healed. Therefore, only antibiotic ointment was used without any coverage. One month after the surgery, the wound was completely healed without any complications (Fig. 6). No residual foreign material was found in tissue sonography.
Discussion
A hot-melt adhesive injected into the finger by a high-pressure glue gun is hard to remove because it undergoes solidification. The temperature of the hot-melt adhesive will generally rise to 120°C. It is known that even a few seconds of contact with a heat source of 60°C will cause second-degree or more severe burn damage [4]. Therefore, injected hot-melt adhesive injuries can cause more severe burns, as observed in our case, than other contact burns with hot-melt adhesive.
In our case, subjective symptoms were not severe after the injection injury, causing the patient to refuse surgical treatment and hospitalization in the emergency room and to also visit the outpatient clinic later than the scheduled date, delaying appropriate treatment. It is known that in high-pressure injection injuries, aggressive debridement within 6 hours can reduce the rates of amputation [1]. In cases of burns due to hot-melt adhesives, the patients’ perception of the burn injury is delayed because of a decrease in skin sensation; there is a study showing that on average the patients’ visit to a hospital for a hot-melt adhesive burn is delayed by 6.6 days [5]. The delayed treatment may do more damage to the burn.
The composition of the injected foreign body is important because many components aggravate the inflammatory response due to direct toxicity, causing further tissue necrosis. High-pressure injections of air, water and small doses of vaccination may need nothing more than observation, and successful outcomes of those injuries have been reported without surgical intervention [6]. However, the most common injections are grease, paint, and hydraulic fluid, in that order [7,8]. The average amputation rate is 30%–48% in high-pressure injection injuries of the hand [1]. Hot-melt adhesives are composed of polymers, tackifiers, and wax components. In industrial hot-melt adhesives, cyanoacrylate is often used to make the adhesive stronger, and can cause chemical burns [9]. While there is no literature on high-pressure hot-melt adhesive injection injuries, they are considered to have a poor prognosis.
It is known that high-pressure injuries to the fingers are likely to confer poorer prognoses because there is less free space in the fingers [10]. Because of the factors above, necrosis progressed more rapidly than expected in the present case, and wound healing was also delayed more than usual.
Initial presentation of high-pressure hot-melt adhesive injection injuries can be deceptively benign, and they are therefore easily overlooked. If the treatment is delayed, sequelae might continue and lead to amputation. The characteristics of the injected material must be identified first. Immediate surgical intervention must follow suit and antibiotic therapy should be accompanied to prevent wound infections. In addition, educating the high-risk population would help to substantially reduce the number of these injuries. Training of emergency room staff and primary care providers is required as well.
Herein, we present a case of high-pressure hot-melt adhesive injection injury. Because initial appropriate treatment was delayed, necrosis progressed more rapidly than expected and wound healing was also delayed more than usual. Our conclusion is that hot-melt adhesive injection injuries are not to be underestimated; immediate surgical intervention should be considered.