Introduction
One of the dressings recently developed to promote wound healing is the bioelectric dressing. From cells in the cardiac conduction system to squamous cells of the epithelium, human cells generate and function through electric signals [1]. In epithelium, this electric field is called the transepithelial potential (TEP) and the typical values for TEP are from 15 to 60 mV [2]. When skin is wounded, this endogenous electric field changes and generates TEP which is crucial for wound healing and cell migration [3]. Procellera (Vomaris Innovations, Chandler, AZ, USA) is a bioelectric dressing that imitates this reaction. This device impregnates small silver and zinc dots in a polyester sheet. A microcurrent is generated when a conductive medium is applied on the sheet. The conductive medium can be the wound's exudate or any other fluid, including normal saline. This chemical reaction occurs by electron transfer from zinc to silver, also known as oxidation-reduction, and does not need external input of power. The process mimics naturally originating electricity within the body and promotes wound healing. It also disrupts biofilm formation and supports cell migration, improving epithelization. While some studies on bioelectric dressings were done in vitro or on animal skin, only a handful of clinical studies were conducted. The aim of this pilot study is to examine the potential effect of bioelectric dressings on skin graft donor sites.
Methods
The study protocol was approved by the Institutional Review Board of Korea University Guro Hospital (No. 2020GR0328). The enrolled patients provided informed written consent. Ten patients were enrolled from November 2020 to July 2021. Primary inclusion criteria were at least 19 years of age, and patients who were scheduled for split-thickness skin graft, with no systemic/local infection sign present at the time of enrollment. Patients who had conditions which could significantly affect wound healing (e.g., connective tissue disease, sickle cell disease, chemotherapy, pregnancy, or those who were breastfeeding) and patients who had allergies to zinc or silver were excluded.
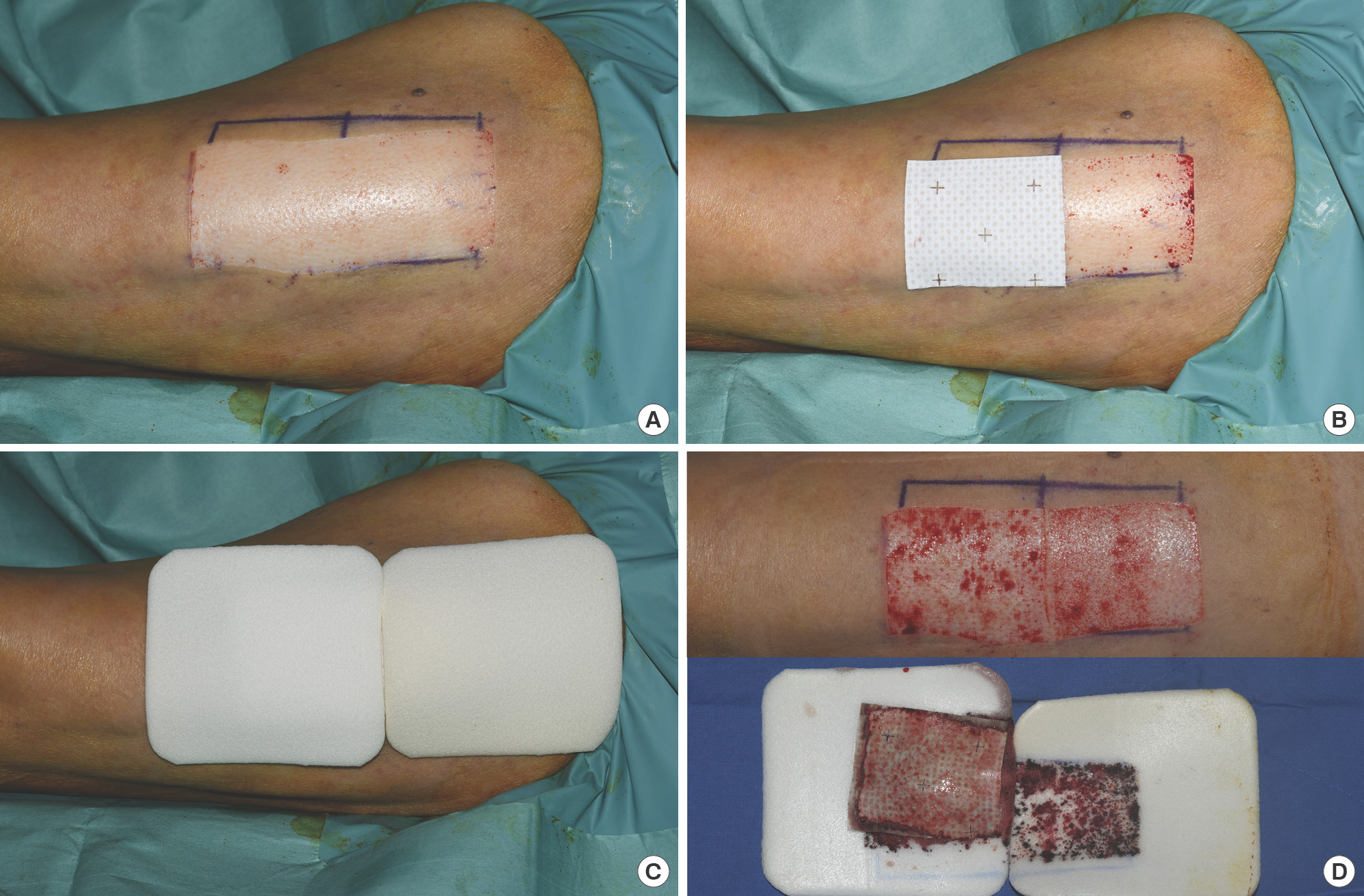
Each patient was sent to the operating room where the third author (SKH) harvested 13/1,000-inch thickness of skin from the lateral upper thigh area using an Electric Dermatome (Zimmer, Keil, Germany). One-half of the donor site was covered with bioelectric dressing (Procellera; Vomaris Innovations) followed by a foam dressing (Mepilex; Mölnlycke Health Care, Gothenburg, Sweden). The other half was covered with only a foam dressing (Mepilex; Mölnlycke Health Care). Five of the patients were administered with bioelectric dressing on the distal portion of the donor site and the others on the proximal portion. Dressings were changed daily for the first 2–3 days to check if the wound was moist enough for the bioelectric dressing to perform. Afterwards, dressings were changed every 2–4 days depending on the exudate of the donor site. Cleansing and irrigation of the wound with normal saline were done whenever the dressings were replaced. A swab culture was done on each portion on postoperative day (POD) 7. On POD 14, each side of the donor site was photographed and evaluated by a blinded plastic surgeon who had more than 30 years of experience in epithelization (Fig. 1).
Results
A total of nine patients successfully completed the study. The patient demographics are provided in Table 1. One patient could not visit the hospital due to personal reasons and dropped out of the study. In terms of epithelization, the bioelectric dressing was superior to the control dressing in seven patients; two of them completely epithelialized on POD 14 and POD 10. The other two cases had similar epithelization ratios on both dressings (Figs. 2, 3).
Table 1.
Patient demographics
| Patient no. | Bioelectric dressing apply site | Sex | Age (yr) | Diabetes | Smoking | Hemodialysis | Result |
|---|---|---|---|---|---|---|---|
| 1 | Distal | Female | 73 | O | Non | O | S |
| 2 | Distal | Male | 63 | O | Non | X | E |
| 3 | Distal | Male | 40 | O | Non | X | S |
| 4 | Distal | Male | 73 | O | Non | X | E a) |
| 5 | Distal | Male | 71 | O | Non | X | E a) |
| 6 | Proximal | Male | 60 | O | Non | O | Drop out |
| 7 | Proximal | Male | 82 | O | Non | X | E |
| 8 | Proximal | Male | 47 | X | Non | X | E |
| 9 | Proximal | Male | 75 | O | Ex | Kidney transplant | E |
| 10 | Proximal | Female | 53 | O | Non | O | E |
Fig. 2.
Case in point (Patient 5). The skin graft donor site was treated with a foam dressing on the proximal (left side in photo) half, and a bioelectric dressing on the distal (right side in photo) half of the wound. Images were taken on operative day (A), postoperative day 5 (B), postoperative day 10 (C), and postoperative day 14 (D), respectively.
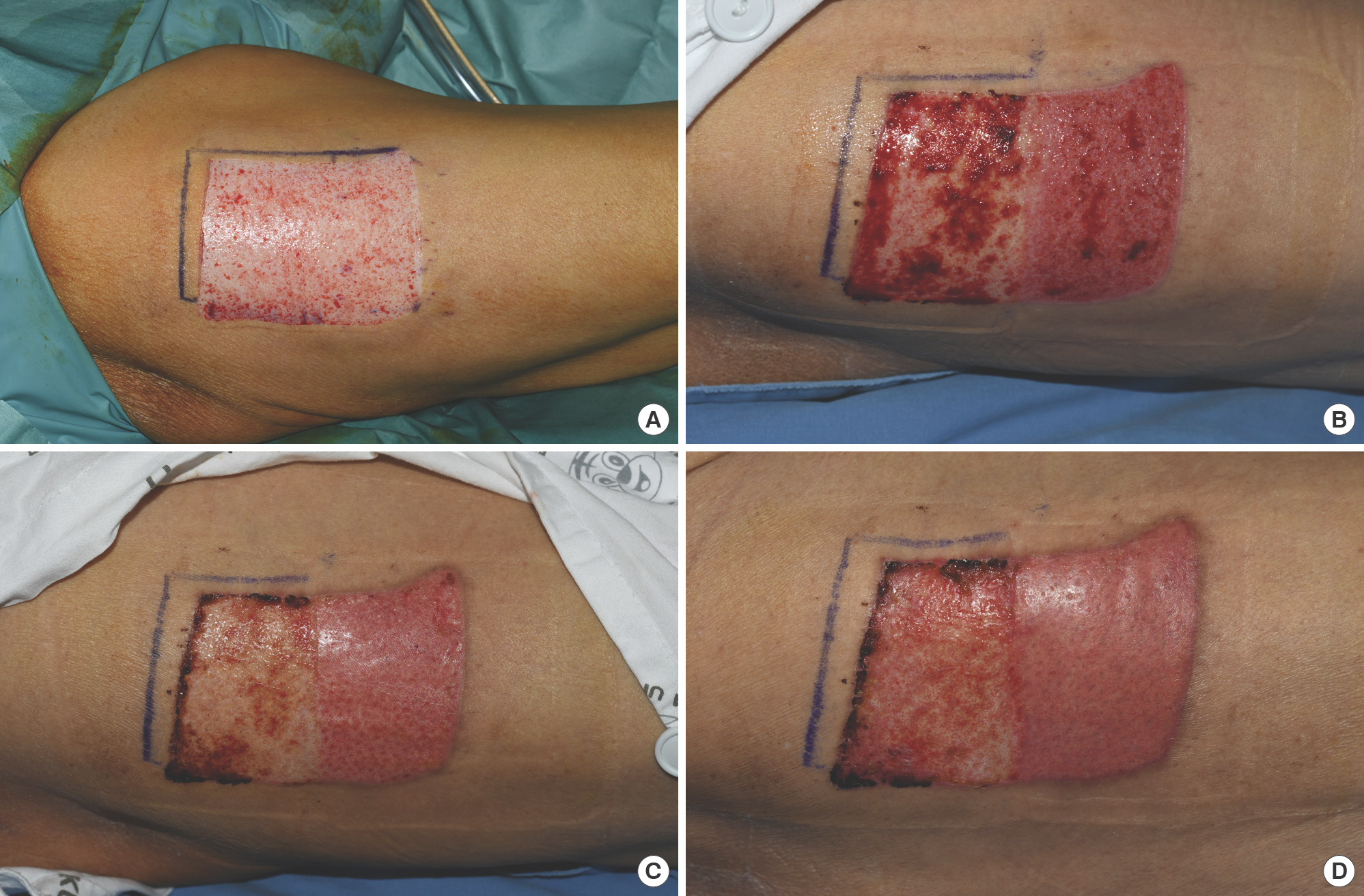
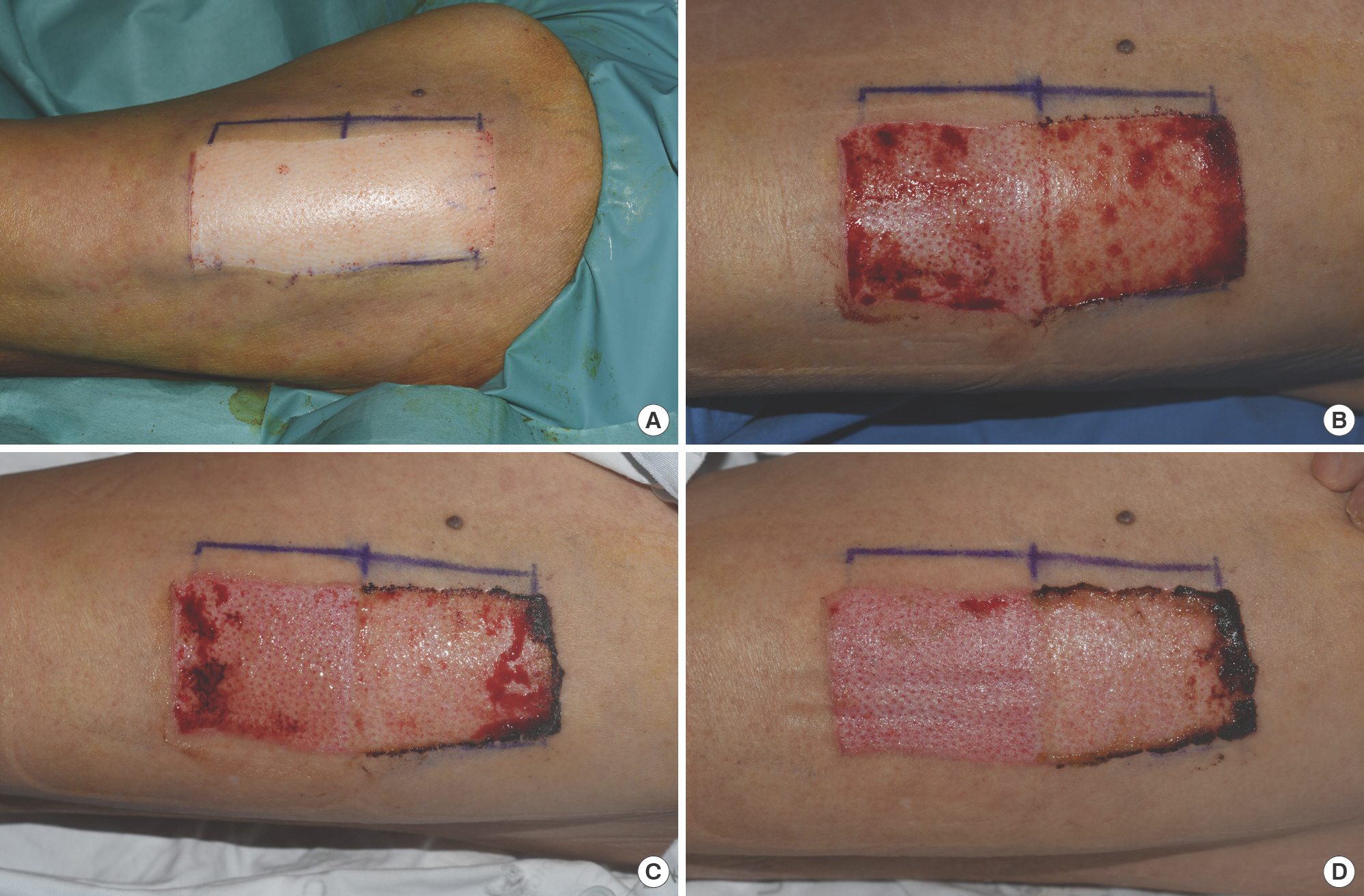
Fig. 3.
Case in point (Patient 4). The skin graft donor site was treated with a foam dressing on the proximal (right side in photo) half, and a bioelectric dressing on the distal (left side in photo) half of the wound. Images were taken on operative day (A), postoperative day 4 (B), postoperative day 7 (C), and postoperative day 10 (D), respectively.
Only one patient had positive results (Staphylococcus epidermidis) from the swab culture on the control side, while all the other swab cultures turned out negative. No complications were observed in any patient.
Discussion
Since the discovery of TEP, investigations have been carried out seeking promotion of wound healing through electrical stimulation. The majority of the researchers tried this method with a device using external sources of power [4]. Further-more, according to a metaanalysis reported by Khouri et al. [5], unidirectional high-voltage pulsed current with active electrodes over the wound provided the best protocol in improving chronic wounds including pressure injuries, diabetic foot ulcers, and venous ulcers. However, patients are not likely to find such external electric devices easy to use. In contrast, the latest bioelectric dressing is not only lightweight but also does not require an external power source, making it convenient for both physicians and patients.
The bioelectric dressing used in this study combines silver and zinc, which generate a microcurrent when added to any conductive medium such as normal saline or any exudate. The bioelectric dressing produces an electric field similar to TEP found in skin wounds, playing a significant role in wound healing. TEP is known to accelerate migration of lymphocytes, fibroblasts, macrophages, and keratinocytes [6–11]. Challenging wounds such as diabetic foot ulcers, venous ulcers and pressure injuries are known to have countless barriers to wound healing. For example, TEP is observed as less active on such wounds and their surrounding epithelium [12]. Keratinocyte migration is especially crucial in epithelization of a wound and is enhanced by electric field energy, which produces hydrogen peroxide (H2 O2), phosphorylates redox-sensitive insulinlike growth factor 1 receptor, reduces protein thiols and increases integrinαν, elevating the mitochondrial membrane potential of keratinocyte which fuels cell migration [3]. Also, the dressing prevents biofilm development by producing superoxide and preventing bacteria from attaching to the wound surface [13]. Moreover, the dressing disrupts quorum sensing by interrupting interbacterial electrical communication. Thanks to these abilities, prior studies using bioelectric dressings showed increase in wound healing compared to standard wound treatment across various types of wounds [14–17]. Infection is always a concern when dealing with chronic wounds; the ability of this bioelectric dressing to disrupt and prevent biofilm formation offers clinicians a strong alternative for care of open and hard-to-heal wounds.
The authors included swab culture to investigate antibacterial efficacy of the bioelectric dressing. One patient showed positive culture results on the control side and negative results on the bioelectric dressing side. This result reaffirms the out-comes of a study by Costerton et al. [18] in which a bioelectric dressing used within 2 hours of the occurrence of an acute wound effectively prevented formation of biofilm. Also, in a study by Barki et al. [19], applying a bioelectric dressing at least twice a week was efficient in eroding biofilm in vivo. Granted, skin graft donor sites are acute wounds which show less development of biofilm than chronic wounds. A positive culture result is when bacteria exceed critical value. While we assumed that the bioelectric dressing might reduce bacterial load compared to the control, our sample size was insufficient to definitively determine culture results. To further investigate the inhibition of biofilm by bioelectric dressings, the authors suggest applying bioelectric dressings on chronic wounds such as pressure injuries or diabetic foot ulcers in later investigations with larger samples.
This study is presumably the first in Korea to investigate bioelectric dressings. The findings of this pilot study confirm the results of an earlier research by Blount et al. [14] that bioelectric dressings help healing of wounds in skin graft donor sites.
This study has the following limitations. First, the bioelectric dressing produces microcurrents promoting wound healing when combined with conductive fluid. Therefore, it is crucial for the donor site to be kept moist. When not sufficiently moist, the polyester-based bioelectric dressing cannot fully perform and causes injury to the wound on removal. Because there was no established protocol to follow, we had to determine the appropriate duration of the dressing treatment and find a way to keep the dressing moist during the investigation. Second, the clinicians who did the dressing in this study were not blinded, and having said that this is a pilot study, there were only a small number of participants. For statistical significance, the subjects should be divided into larger groups by specific illness (e.g., diabetes). Third, cost-effectiveness of the bioelectric dressing was not considered in this investigation. In clinical settings, in addition to wound-healing properties and antibacterial function, cost-effectiveness is a crucial factor in choosing a dressing material. The authors hope further studies are conducted taking cost-effectiveness into consideration with larger sample sizes.