Introduction
The coverage of defects in the anterior lower leg is often challenging and difficult for reconstructive surgeons because of relatively insufficient soft tissue compared to other areas of the lower leg [1,2]. This inherent feature of the anterior lower leg makes the coverage of even a small defect difficult, resulting in the exposure of underlying structures (e.g., tendons and bones) [1,2]. Today, free-flap surgery is a valuable reconstructive tool for covering defects in the lower extremities, given recent advancements in microsurgical concepts and skills [2,3]. However, free-flap surgery requires several conditions, including skilled microsurgeons, the hospital’s capacity to support microsurgical operation and care, and the patient’s ability to bear microsurgery [2,4-6]. This means that other reconstructive modalities (e.g., skin grafting and local flaps) are still useful in lower extremity reconstruction. Particularly, local flaps can be the primary choice for coverage in some cases and are applicable as an alternative to free tissue transfers in lower extremity reconstruction [2,5]. This study presents the experience of using the keystone flap (KF) with omega variation (OV) [7] and Sydney melanoma unit modification (SMUM) [8] for covering small- to moderate-sized defects in the anterior lower leg. The main purpose of the present study is to substantiate the practical and versatile application of OV and SMUM KF in lower extremity reconstruction.
Methods
The study involved patients who underwent KF reconstruction with OV and SMUM to cover defects in the anterior lower leg from December 2017 to June 2020. Patients who underwent only KF reconstruction, i.e. only the OV KF, only the SMUM KF, and a combination of the OV and SMUM KF, were included. However, patients who underwent anterior lower leg reconstruction using other types of KF, such as type I (skin incision only), type II (a division of the deep fascia), type III (opposing KFs designed to create a double-KF), and type IV (KF with undermining of up to 50% of the subfascial flap) [9] were excluded. Data from the patients’ medical records and clinical photographs, including cause of defect, defect location, defect size, flap size, KF type, flap survival, postoperative complications, and follow-up period, were retrospectively reviewed and evaluated.
This study was approved by the Institutional Review Board of Konyang University Hospital (approval number: 2017-07-004). Moreover, all research procedures in this study were performed following the ethical guidelines of the 1975 Declaration of Helsinki. All participants provided written informed consent.
Surgical techniques
Each patient received preoperative management for wound preparation, including serial debridement, conventional wound dressing, negative-pressure wound therapy, and antibiotic treatment to control infection and inflammation of surrounding tissues, for at least 1–2 weeks. The final defect was covered with the KF technique with OV and SMUM after achieving wound preparation and stabilization through these treatments. The operation was performed in the supine position and under local or general anesthesia, depending on the size of the defect and the patient’s general condition. The final defect was measured after complete debridement. Consequently, we tried to check and mark perforator hotspots around the defect using a handheld ultrasound Doppler device as much as possible, especially in larger defects. Both the size of the defect and laxity of surrounding tissue were considered when designing the flap [2,5,6]. The width of the flap was designed to be larger than that of the defect, and the flap center was located on the marked perforator hotspots [2,5,6].
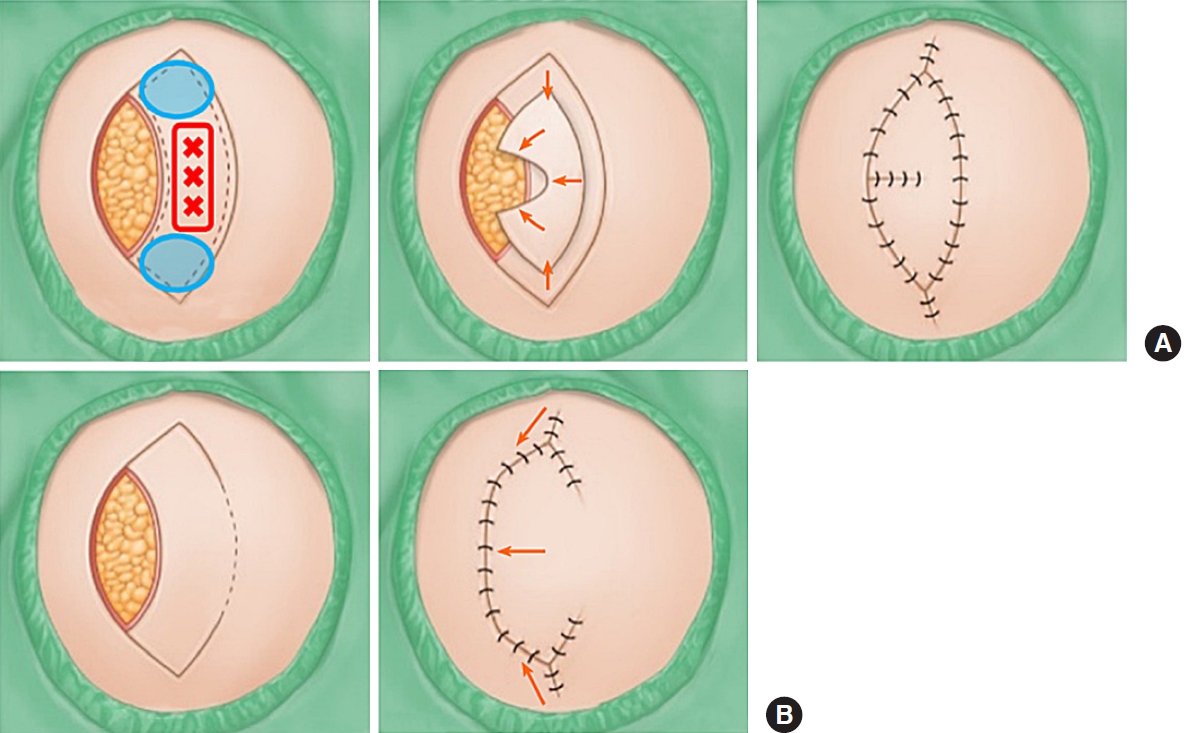
Either OV KF alone, SMUM KF alone, or a combination of OV and SMUM KF was used for each case. OV KF was used to add rotational flap movement. The original defect was therefore closed in a fish mouth fashion [5-7]. SMUM KF involves the maintenance of a skin bridge along the greater KF arch [5,6,8]. Basically, we used the SMUM KF in case of either smaller defects or imprecise perforator hotspots found in Doppler tracing, and used the OV KF when there was need for further flap movement to achieve tensionless closure. The modification was decided intraoperatively instead of preoperatively; specifically, the initial skin incisions were performed with the maintenance of a skin bridge along the greater KF arch (SMUM), and then could be converted into OV (extension of incision through the skin bridge) according to intraoperative findings. Fig. 1 illustrates OV KF and SMUM KF. A skin incision was created along the flap, and dissection was done from the subcutaneous layer to the deep fascia. A skin bridge along the greater arch of the KF remained when SMUM KF was applied. Minimal undermining of the flap margin was performed to preserve vascular perfusion of the central perforator hotspot [2,5,6]. This procedure should only be done to the extent that the flap is moved toward the defect in either linear or OV closure with minimum tension. After meticulous hemostasis, the flap was inserted in the following sequence: first, the defect side of the flap was sutured in either linear or OV closure, followed by both ends of the flap in a V-Y closure fashion; second, the donor site of the flap was sutured; and lastly, a mild compressive dressing with foam materials was applied.
Results
The study included six patients (four men and two women) with an average age of 41.67±22.42 years (range, 14–70 years). Table 1 summarizes the patients’ characteristics and clinical data. The defects’ etiology included skin necrosis due to trauma in five patients, and skin necrosis from burns in one patient. The defects’ locations included the lower third of the anterior lower leg, the middle third, and the upper third in two, three, and one patient, respectively. The defect and flap sizes ranged from 1.5×2.5 to 6×8 cm and 3×6 to 8×17 cm, respectively. Using handheld ultrasound Doppler tracing intraoperatively, precise perforators were obtained for two patients. Four defects were covered using OV and SMUM KF, one defect was covered using SMUM KF, and another defect was covered using OV KF combined with an additional tiny skin graft. All flaps remained completely viable without flap-related complications (e.g., venous congestion, arterial insufficiency, or partial flap loss). Only one case (case 4) showed maceration of part of the flap margin; it was not a fully broken wound, but healed incompletely with partial wound dehiscence at the time the stitches were removed. The maceration was mitigated with conservative dressing and did not require further surgery. There was no development of other postoperative complications such as hematoma, seroma, or wound infection. After an average follow-up period of 4.83±1.17 months (range, 4–7 months), no recurrences or problems exist at the operative sites. Furthermore, all patient outcomes were satisfactory.
Case presentations
Case 1
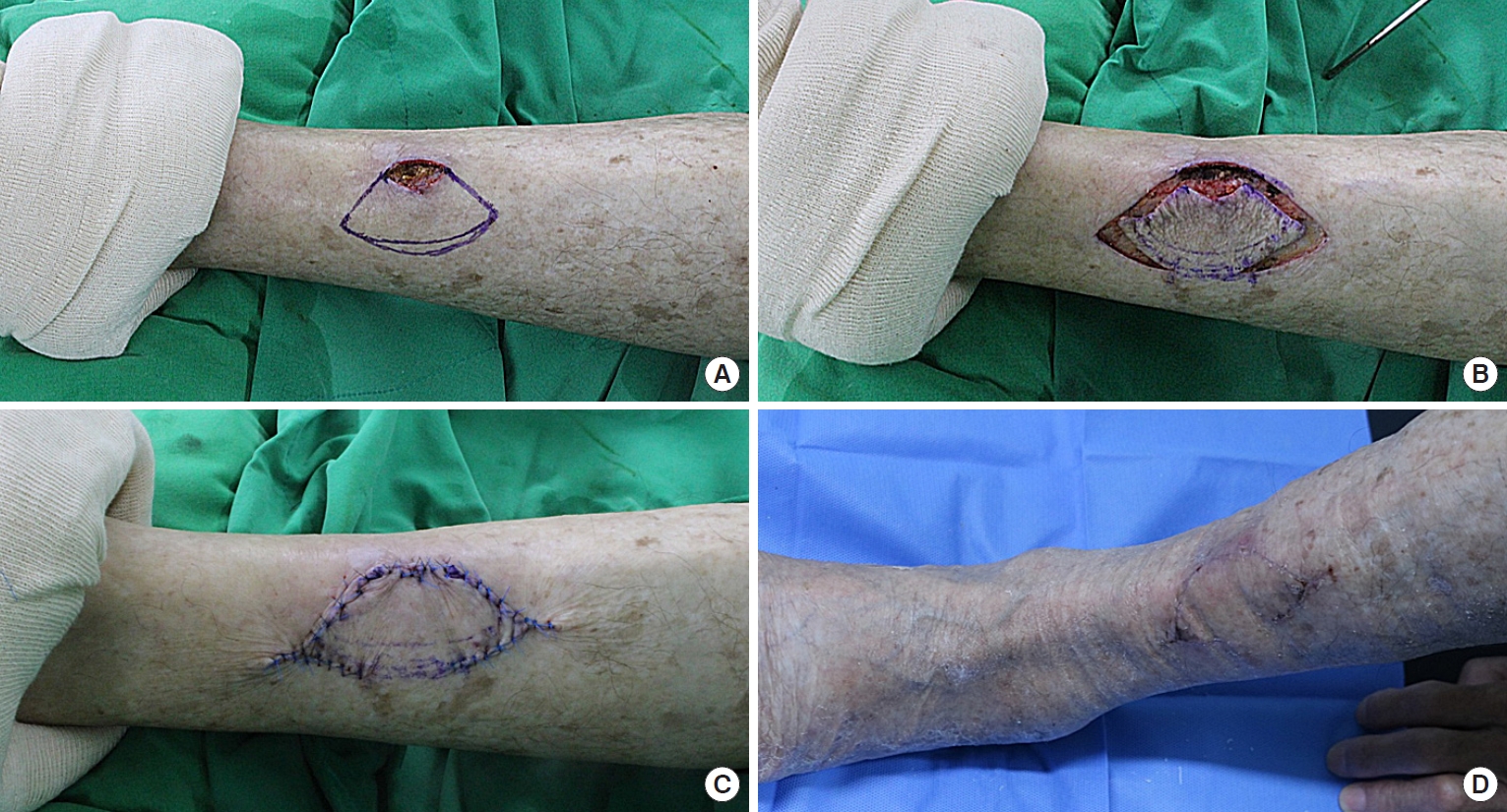
A 70-year-old man suffered from skin necrosis on the lower third of the left anterior lower leg (Fig. 2). Wound preparation procedures, including serial debridement, conventional wound dressings, and empirical antibiotic medication, were performed for one week. The final post-debridement defect size was 1.8×4 cm. The defect was covered with SMUM KF (3.5×7.5 cm) from the defect’s lateral side. The flap remained completely viable without any postoperative complications. The patient showed favorable outcomes and was satisfied with the result at 5 months follow-up.
Case 3
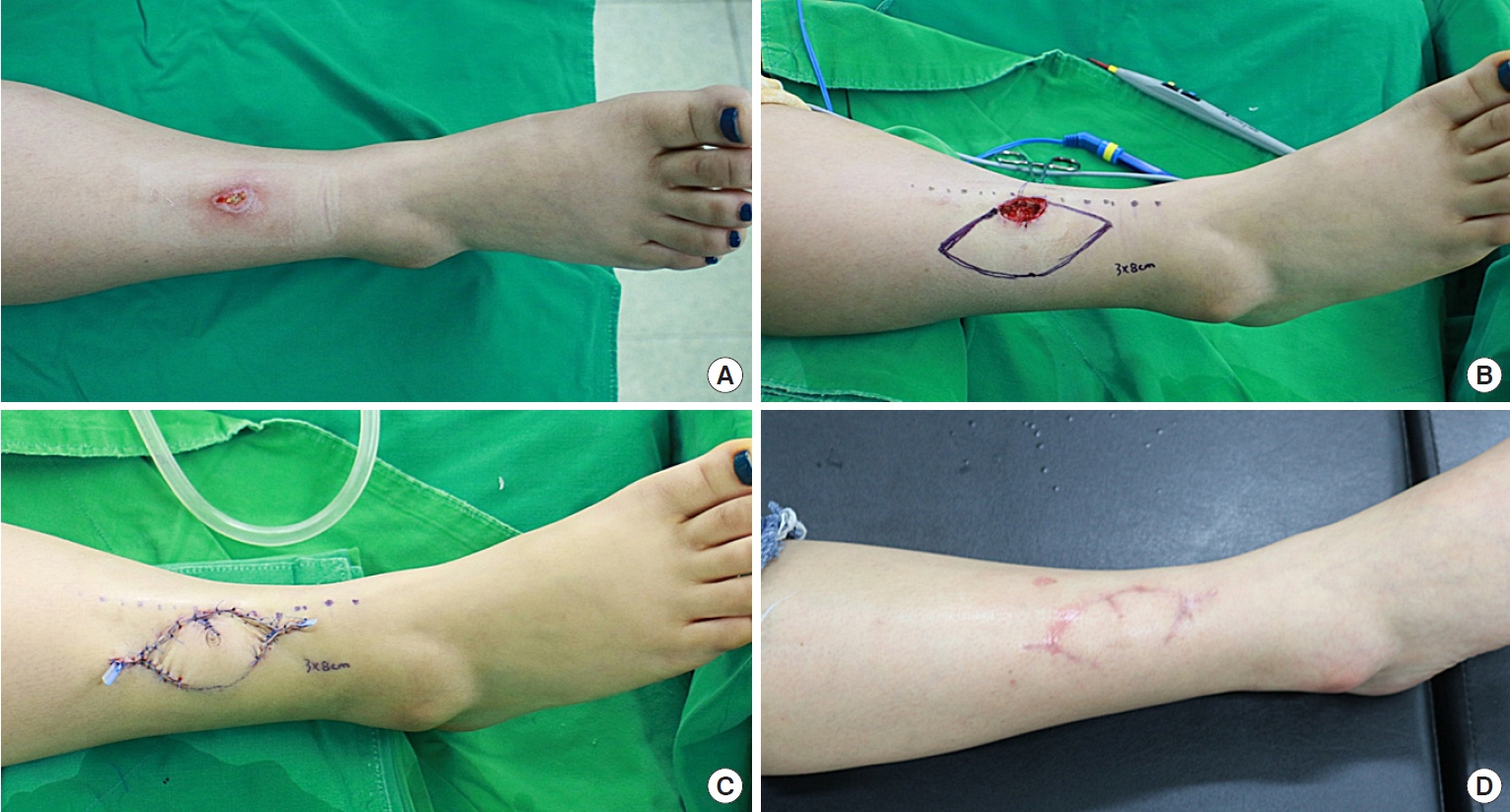
A 28-year-old woman suffered from skin necrosis on the lower third of the right anterior lower leg (Fig. 3). Wound preparation procedures, including serial debridement, negative-pressure wound therapy, and empirical antibiotic medication, were performed for one week. The final post-debridement defect size was 1.8×3.5 cm. The defect was covered with an OV and SMUM KF (3.5×8 cm) from the lateral side of the defect. The flap was completely viable without any complications. The patient showed favorable outcomes and was satisfied with the result at 7 months follow-up.
Case 5
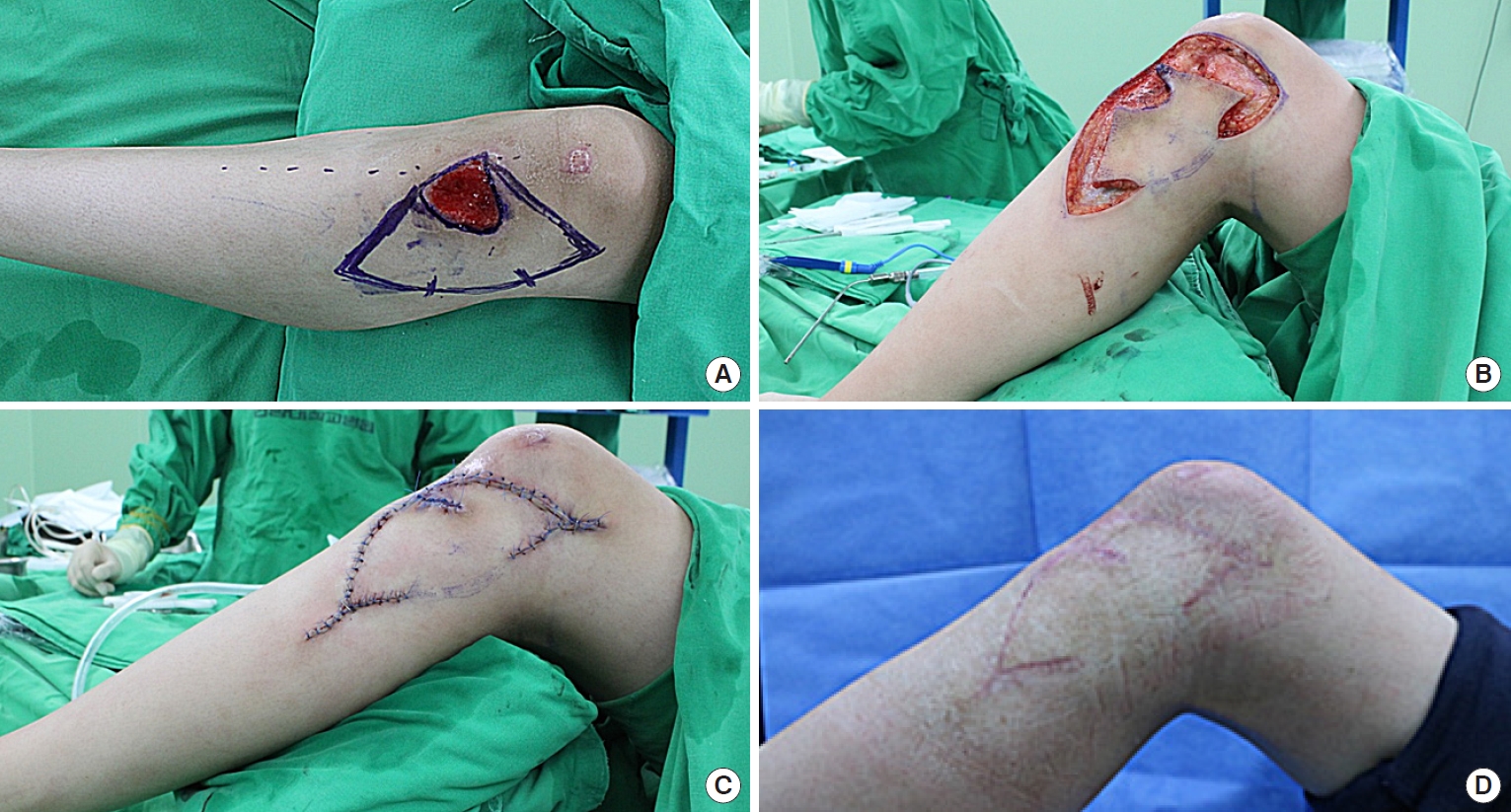
A 14-year-old male teenager suffered from a skin avulsion on the upper third of the left anterior lower leg (Fig. 4). Wound preparation procedures, including serial debridement, conventional wound dressings, and intravenous antibiotic therapy, were performed for two weeks. The final post-debridement defect size was 3×4 cm. The defect was covered with an OV and SMUM KF (5×12 cm) from the lateral side. The flap was completely viable without any postoperative complications. The patient had a favorable functional outcome without limitations to knee joint motion. However, at 5 months follow-up, there was mild hypertrophic scar formation, even though the patient had used CICA-CARE for postoperative scar management.
Discussion
The present study described the experience of successfully utilizing the OV and SMUM KF technique to reconstruct six consecutive cases of anterior lower leg defects, conducted by a single surgeon (the corresponding author of this study). As previously stated, reconstruction of anterior lower leg defects is always troublesome and challenging [1,2]. This is particularly true because the anterior lower leg includes pretibial regions, which are nearly bone-to-skin, lack underlying tissues, and have limited tissue mobility [1,2]. Therefore, local flap reconstruction is limited, and great care should be taken to apply local flaps in the anterior lower leg [2]. Large anterior lower leg defects may inevitably require free-flap coverage. In contrast, local flap techniques can be a good alternative modality for small- to moderate-sized defects in the anterior lower leg [2]. The present study successfully covered anterior lower leg defects of up to 6×8 cm in size with OV and SMUM KF technique. Meanwhile, a skin graft is a feasible reconstructive option for anterior lower leg defects exhibiting a healthy granulated wound bed without exposure of underlying structures. However, it has definite disadvantages including other donor-site morbidity, secondary contracture, color mismatch, and contour deformity. The disadvantages prevented the clinicians from considering skin grafts for the majority of the cases in this study.
Though conventional muscle-based local flaps (e.g., soleus, gastrocnemius, and tibialis anterior muscle flaps) have been used for anterior lower leg defects [2], they are usually accompanied by functional deficits, marked donor-site morbidities, or poor aesthetic outcomes [2]. More recently, pedicled perforator flaps (PPFs), in the form of propeller and island flaps, have changed the paradigm of lower limb reconstruction in terms of liberty and flexibility of flap design, decreased donorsite morbidity, and provision of like-with-like tissue type [2,5,10]. Several previous studies have demonstrated the PPF reconstruction of lower extremity defects [2,10]. PPFs (e.g., peroneal artery, medial sural artery, and posterior tibial artery perforator flaps) are known to cover 75% of the lower extremity’s total surface area from the superior patella to the forefoot [10]. Literature also reports that each flap could cover defects around the lower leg, ranging from 15% to 26% of the surface area [10]. Moreover, PPFs are easier to perform and entail less risk than free-flaps as they do not require microsurgical anastomosis [2,5,10]. Nevertheless, microsurgical abilities such as the perforator dissection technique and venous supercharging technique are still critical in PPF reconstruction [2,5,10]. For residents or novice reconstructive surgeons who lack training in these techniques, simpler flap techniques (e.g., perforatorbased island flap devised by Kim et al. [11] and KF) are a useful alternative [2,5,6] because they do not require microsurgical perforator dissection [2,12]. Furthermore, no microsurgical skills were used in any of our cases.
The KF is one type of perforator-based flap devised by Behan in 2003 [9]. It is a multiple perforator-based advancement flap with a curvilinear trapezoidal shape, designed to mimic the keystone in Roman arches [9]. Moreover, KF has gained popularity over the last 20 years as a meaningful innovation in reconstructive surgery and has been applicable as either a primary or an alternative reconstructive method [2,5,6]. A variety of studies have described the utility of KF reconstruction to cover diverse defects in almost every part of the body [2,5,6,13]. KF has also been used in lower limb reconstruction, mainly after skin and soft tissue tumor resection in the thigh and calf regions [2,14]. The vast majority of previous studies demonstrated KF reconstruction in the lateral and posterior lower extremities, which typically have sufficient tissue volume for recruitment. However, only a few studies have applied the KF for anterior lower extremity reconstruction [2]. A previous study conducted by the present study’s senior author group demonstrated a successful case series of traumatic pretibial defect reconstruction using KF [2]. It emphasized that while KF may not be the primary flap of choice for covering pretibial defects, it can still be a good alternative to other reconstructive options in selected cases [2]. The present study, an extension of the previous study, focuses on the effectiveness of OV and SMUM KF for covering small- to moderate-sized defects in the anterior lower leg.
The KF consists of double-opposing V-Y flaps joined together; their advancement toward the flap center (along the longitudinal axis) provides some residual laxity within the flap, which allows for KF movement into the defect (along the horizontal axis) [2,5,6]. Fundamentally, the gradual release of tissue layers, including skin (especially dermis), superficial fascia (subcutaneous layer), and deep fascia during flap dissection promotes KF movement [6,15]. Additionally, minimal undermining of the flap margin provides additional flap movement [2,5,6,13,15]. Particularly, these biomechanics form the basis of the KF movement and result in the principal recruitment of tissue laxity in KF reconstruction [5,6,15]. Namely, KF reduces wound tension through recruitment and rearrangement of tissue laxity [5,6,15]. Securing minimal wound tension when covering defects is crucial because there is insufficient surrounding tissue in the anterior lower leg [5]. Attempts for classical KFs without any modifications may encounter difficulties covering the anterior lower leg defects due to the aforementioned inherent feature.
From these perspectives, both OV and SMUM are very useful modifications in the KF reconstruction of the anterior lower leg. OV KF provides further flap movement via additional rotational movement, further reducing tension without sacrificing the healthy tissues in wound closure [2,6,7]. Meanwhile, SMUM KF allows additional vascularity and provides structural stabilization of the flap by maintaining a skin bridge along the greater arch of the KF [2,6,8]. The KFs’ complete viability, with no flap-related complications, was achieved in the present study by applying OV and SMUM in all cases. Also, there were no significant complications, and all patients experienced favorable outcomes. Meanwhile, the present study did not establish a specific range for the size of the defect to qualify for KF reconstruction. The smallest defect among the current study cases was 1.5×2.5 cm, which could be considered adequate to achieve primary closure with undermining or bilateral skin flap advancement [15]. However, as each patient has different skin properties, some small defects may achieve ineffective primary closure when there is a certain level of wound tension and persistent dead space, possibly causing obstacles to the wound healing [15]. The skin properties of each patient and characteristics of surrounding tissues should be considered when determining the effectiveness of flap reconstruction for covering defects [15]. Furthermore, KF reconstruction was performed in all cases in the present study because the authors believed that it would be effective in minimizing wound tension in the anterior lower leg, which would facilitate the postoperative wound healing process with minimal complications.
This study has some limitations despite its successful results. First, the present study is a nonrandomized retrospective clinical review with very small sample size and no comparison group [2,5,13], meaning that some selection bias and confounding factors inevitably exist. Further prospective large-scale studies are required to confirm consistently favorable outcomes [2,5,13]. Second, OV and SMUM KFs cannot be the only solution for anterior lower leg defects as other local flap techniques can also achieve good results, depending on the specific conditions of each wound. It is important that surgeons determine the best method to ensure the most favorable outcome for each case [6]. Third, compared to linear scars in primary closure with undermining, KF reconstruction inevitably extends operation scars [6,15]. Furthermore, the KF presents a larger flap size with longer incisions than other conventional local flaps (e.g., the Limberg, rotation, and transposition flaps) [6,15]. Additionally, dog-ear deformity in both ends of the KF and cone deformity in the OV KF can occur, which results in less aesthetically pleasing outcomes [6]. Therefore, surgeons should explain thoroughly the possibility of extended scar formation to patients undergoing KF reconstruction and stress the necessity for longer postoperative scar management [6,15].
This study successfully covered small- and moderate-sized anterior lower leg defects with OV and SMUM KF with favorable outcomes. Based on the present study experience, the OV and SMUM KF techniques are considered good alternative modalities for anterior lower leg reconstruction.