Introduction
Prolonged pressure on the ischium in nonambulatory patients often causes ischial ulcers. A pressure ulcer usually starts as a small superficial wound, but without adequate management, becomes deeper and eventually requires surgical repair [1]. In patients with wound infections, poor nutrition, and uncontrolled chronic diseases, surgical repair may have to be delayed until their condition improves, and surgery might never be performed in extremely ill patients. In such patients, open wounds are often challenging to manage with conventional dressing methods because they generally produce a profuse exudate, involve a large sinus cavity, and are easily contaminated from the neighboring anus. In order to effectively manage intractable ischial wounds, we devised a closed irrigation system using the Barovac (50–90 mmHg) wound drainage device and a saline infusion set and applied the system to a 50-year-old paraplegic patient with a complicated ischial ulcer. This system contributed significantly to keeping the patient’s ischial wound clean until his general condition improved and surgical repair could be undertaken. In this study, we describe our closed irrigation system for managing complicated ischial wounds. This study was approved by the Institutional Review Board (IRB) of Kangwon National University Hospital (IRB No. KNUH-2020-09-009-002). The patient provided written informed consent for the publication and the use of his images.
Ideas
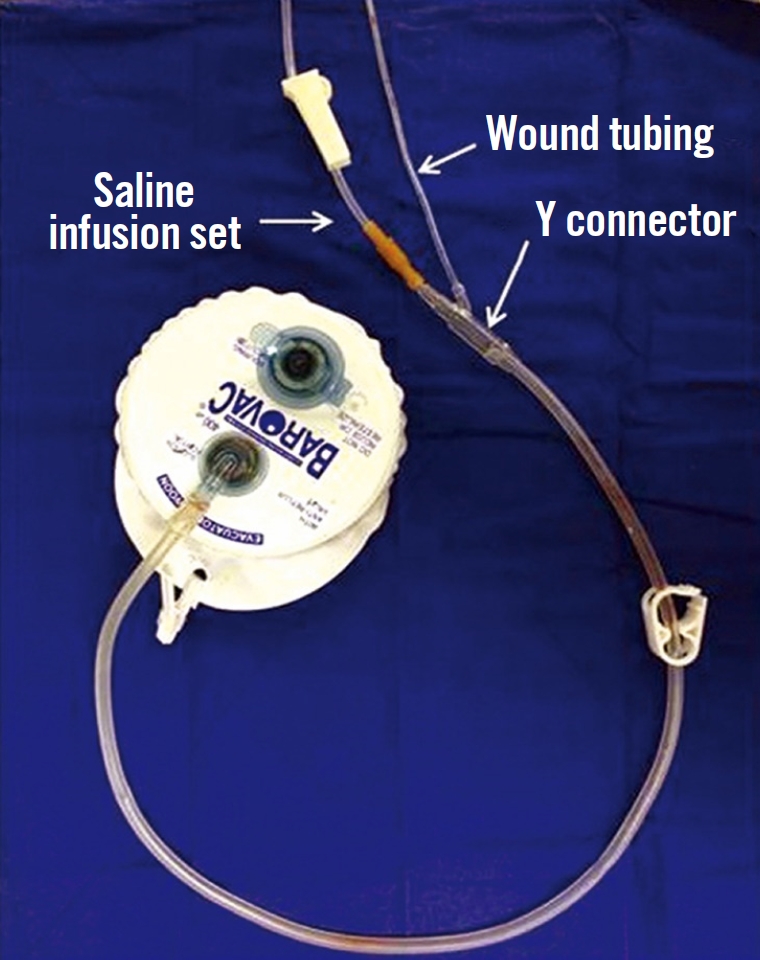
A 50-year-old paraplegic man was admitted due to a longstanding deep ischial ulcer accompanied by a high fever. The ischial open wound showed a large sinus cavity extending to the vicinity of the anus along with a profuse discharge (Fig. 1). Since the patient’s vital signs and laboratory results were consistent with a clinical diagnosis of impending sepsis caused by secondary infection superimposed on the ischial ulcer, intravenous administration of vancomycin and piperacillin/tazobactam was started after performing wound and blood culture tests on the recommendation of an infectious disease specialist. On the 2nd day after admission, the ischial open wound was profusely irrigated with a saline solution in the operating room, followed by direct closure along with debridement of the margin after inserting the wound tubing of a Barovac (Sewoon Medical, Seoul, Korea) wound drainage device in the ischial cavity. The main tip of the Y connector at the end of the evacuating tube of the Barovac wound drainage device, after having been cut short, was connected to the rubber connector of a saline infusion set, while the side tip of the Y connector was connected to the wound tubing (Fig. 2). In the ward, 200 mL of saline was infused every 6 hours through the saline infusion set, and fluid in the wound cavity, including exudate and debris, was evacuated continuously through the wound drainage device after a 10-minute dwell time by nursing staff (Fig. 3). The evacuating tube was locked during saline infusion, and the saline infusion set was locked during evacuation. Wound management was maintained using this system until the general condition of the patient improved. Subsequently, surgical repair using the internal pudendal artery perforator flap after radical debridement and bursectomy was performed in the 2nd week.
Discussion
Wound dressing plays an important role in wound healing and management. Over the past several decades, the concept of wound dressing has changed. Today it focuses on promoting wound healing as well as wound protection. Consequently, moist dressing and negative-pressure wound therapy (NPWT) have been introduced and are widely used to manage various wounds. NPWT, also known as a vacuum-assisted closure, is an established treatment option to remove excess exudate and promote healing in acute or chronic wounds. Negative pressure is understood as aiding wound healing through a number of mechanisms including macrostrain, microstrain, fluid removal and optimizing the wound environment [2]. For management of complex wounds with infection, NPWT with instillation and dwell time (NPWTi-d) can be used as adjuvant therapy along with appropriate debridement and antibiotic therapy [3]. This therapy can control the range of fluid instillation and irrigation and has been reported to overcome some limitations of standard NPWT [4] by delivering topical wound solutions directly to the wound, according to conditions set by the physicians. It therefore allows the solution to dwell over the wound bed, and removes the solution during the negative pressure phase [3]. This device was proposed to enable complete wound bed preparation even in relatively severe conditions such as infected wounds or exposure of bone or tendon [4].
Wound irrigation is an essential part of wound management, and is used to remove foreign material, reduce bacterial burden, and remove cellular debris or exudate from the surface of the wound [5]. The benefits of regular wound cleansing with a topical solution in NPWT have become more apparent in recent years, especially for addressing impediments to healing [6]. Various topical solutions have been applied for this purpose; a recent study demonstrated that instilling normal saline achieved comparative outcomes as with other antiseptic solutions [7]. Other case series have also reported successful outcomes with saline [8,9]. While NPWTi-d can also be considered for the management of complicated ischial ulcers accompanied by profuse discharge due to secondary infection (as in our case), it is difficult to apply the dressing kit and maintain an occlusive dressing in the ischial area. Therefore, our system can be used as an alternative to NPWTi-d. We also observed that wound cleansing with the regular instillation of saline in our system contributed to better wound management.
The system we employed has several advantages over traditional wound dressing methods. Firstly, the dressing is very convenient because the open wound has already been closed. Secondly, secondary infection from fecal contamination can be prevented. Thirdly, using the proposed approach prevents the bedsheets and clothes of the patients from becoming wet. Further, our system is easily applicable and inexpensive. Although our research is insufficient for establishing guidelines for our system, we suggest a 100–200 mL saline infusion every 6 hours, followed by continuous drainage with 50–90 mmHg of negative pressure after a 10-minute dwell time. The amount of saline infusion depends on the size of the wound cavity. Meanwhile, the instilled solution should be allowed to dwell in the wound so that it has adequate time to cleanse the wound [10]. Though appropriate instillation dwell time has been proposed at 10 minutes [6], the dwell time and intervals between saline infusion can be adjusted according to the wound conditions. Alternatively, our system can be easily modified by adding a medical three-way stopcock to the saline infusion tubing when infusion of an antiseptic solution is needed in the wound cavity.
Wound debris often causes clogging of the wound tubing. A squeezing technique or passage of a fine cannula can help clear the blockage. For intractable blockages, the wound tubing can be easily replaced with new tubing through a small incision in the previous wound closure site. When replacing old tubing, microbial culture for its tip may be considered.
Our system has limited indications; in particular, it should only be applied to open wounds that can be closed directly. Nevertheless, we argue that our closed irrigation system using the Barovac wound drainage device and a saline infusion set can help keep wounds clean and prevent secondary infection not only in patients with complicated ischial ulcers, but also in chronically debilitated patients with irreparable ischial sores.