Introduction
Electrical burn injuries are generally more severe than thermal injuries. Electrical burns often extend into the subcutaneous tissue and cause necrosis of the muscle, tendon, and bone. Moreover, electrical burns can occur at multiple sites and cause deep wounds [1,2]. Electrical burns extending to the bone complicate reconstruction. Treatment of electrical burns mainly employs complex flaps such as free flaps, as skin grafts do not take readily because the soft tissue is insufficient [3-5]. Multistage reconstruction is often required. In particular, as severe electrical burns on the lower extremities can cause functional impairment, it is important that appropriate treatment is provided to accelerate the recovery. We present a case in which an electrical burn patient with multiple fourth-degree burns was treated with an alternative method when severe vessel thrombosis made flap surgery dangerous. The study was approved by the local ethics committee of Hanil General Hospital (approval No. HGH-2020-OTH-004). This study adhered to the ethical principles outlined in the Declaration of Helsinki and the patient provided written informed consent for the publication and the use of his images.
Case
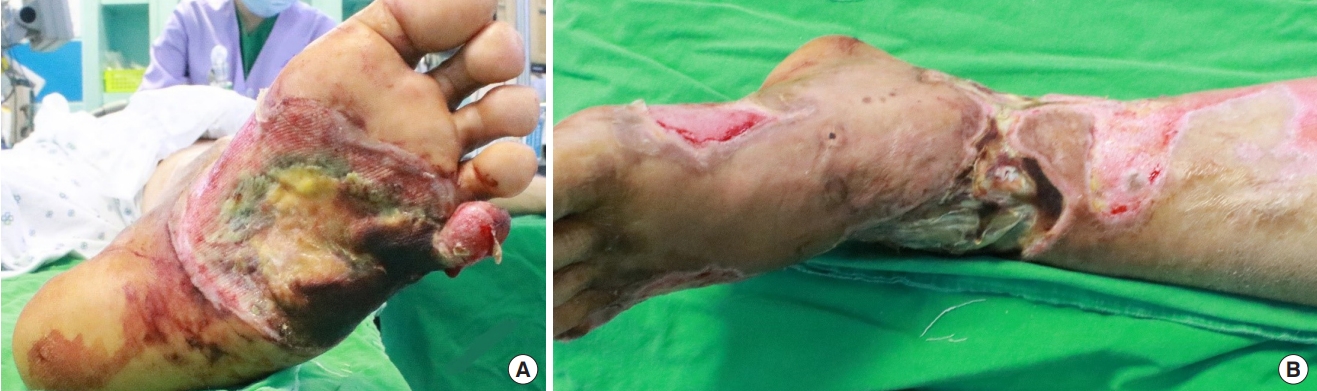
A 56-year-old man was injured by a 15,000-V electrical current. The entry site was his right hand and exit site was his left foot. The entry site showed a 1.5×1 cm circular third-degree burn on his palm. A dried black eschar was observed on the medial side of the left ankle, while the skin on the lateral side of the plantar was notably pale and dry. The plantar wound included a soft tissue defect, thick central eschar, and mottled lateral tissue (Fig. 1). The patient initially presented with signs of rhabdomyolysis but no signs of cardiac problems.
Observing severe tissue destruction, we planned serial debridement and negative-pressure wound therapy (NPWT) to stimulate formation of granulation tissue and facilitate healing of the wound.
Debridement was performed 5 days after the injury, and NPWT was administered the day after debridement. When we first debrided the wound, the eschar had encircled the patient’s left ankle and the lateral side of that foot was mummifying. Soft tissue defects and an enlarged necrotic area were observed on the plantar wound (Fig. 2).
On exploration, the tendons and muscles were nonviable and the underlying vessels showed thrombosis. The tibial cortex was desiccated and the 4th and 5th metatarsals were completely burned. We debrided the third to fifth extensor digitorum tendons and the adjacent muscles and nerves. The tendons and parts of muscles of the tibialis posterior and flexor digitorum longus were debrided. We amputated the 4th and 5th metatarsals as well as the 5th toe; we also burred into the outer table of the exposed tibia. We performed wide debridement with bone burring and changed NPWT several times over 3 to 4 days (Fig. 3). Following the 8th administration of negative wound therapy, we performed skin grafting using one-stage acellular dermal matrix (AlloDerm, Lifecell Corp., Branchburg, NJ, USA) on both sides of the ankle and on the plantar side 7 days after primary skin grafting. The graft site healed at around 10 days after surgery.
The multiple wounds healed within 56 days after the burn injury. The patient could stand on his own; however, because he could not flex or extend his ankle, he experienced discomfort while walking (Fig. 4). He was transferred to rehabilitation medicine where he practiced exercising and walking. At the 1-year follow-up, he could walk independently wearing a splint to prevent ankle drop (Fig. 5). A second soft tissue reconstruction could be considered if the patient shows any signs of discomfort, such as chronic ulcers or pain.
Discussion
Burn wounds caused by electrical injury can be direct or indirect; direct injury is thermal damage from the heat generated by high voltages, and indirect injury is due to vascular injury and the prolonged production of thromboxanes induced by the electrical current [1,2]. As with vascular injury and vascular thrombosis, the tissue destruction caused by electrical burns is often progressive, worsening with time.
As electrical burns cause large soft tissue defects and extend to underlying fascia, muscle, tendon, and bone, they present complex reconstructive problems. Multistage reconstruction is often required, with various methods used for reconstruction. Free tissue transfer is recommended for burns with exposed tendons, bones, and vital organs [4,5]. However, this may not be appropriate if the vessels are unstable. Multiple, large donor site defects may increase morbidity and further cause functional impairment of the donor site itself, leading to new problems.
In our case, the patient had multiple severe burns on his ankle and plantar area. He had injured muscles, tendons, and bones in all wounds, and the wounds had thrombosed vessels at multiple sites. We decided that the vascular risk for a free tissue transfer operation would be too high because of latent injury to the intima of the surrounding vessels, and that regardless of the method used for tissue reconstruction, his ankle would have minimal function after the wound had healed. Therefore, for the primary stage, we planned for reconstruction without loss of soft tissue or function in other parts of the body. The primary aim was proper healing and preserving the foot to support the body. We planned to transfer or supplement soft tissue in the next operation if the patient had trouble walking. To obtain sufficient soft tissue for wound healing, we used burring and NPWT. Burring into the vascularized medulla of the bone has been known to stimulate granulation [6,7]. NPWT has been proved to generate sufficient amounts of granulation tissue, even in areas where bone was exposed [8,9]. We therefore performed serial wide debridement of the necrotic tissue and then used NPWT to stimulate granulation with a subsequent split-thickness skin graft.
The patient healed at approximately 56 days after the burn injury and experienced satisfactory functional recovery. After exercising in rehabilitation for a while, he was able to walk with the assistance of a cane. To help him walk, we decided to consult the rehabilitation medicine center to construct a splint to prevent his ankle from dropping. At the 1-year follow-up, he was able to walk on his own in the splint. Secondary soft tissue reconstruction could be considered if the patient experiences discomfort due to development of a chronic ulcer or suffers from pain.
The treatment of choice for serious wounds with exposed bones is flap surgery. However, this may be too much of a risk when multiple flaps are required and the blood vessels are damaged, and an alternative should be considered. We look forward to reporting more cases with favorable results using NPWT in patients at high risk of flap surgery with multiple fourth-degree burns.